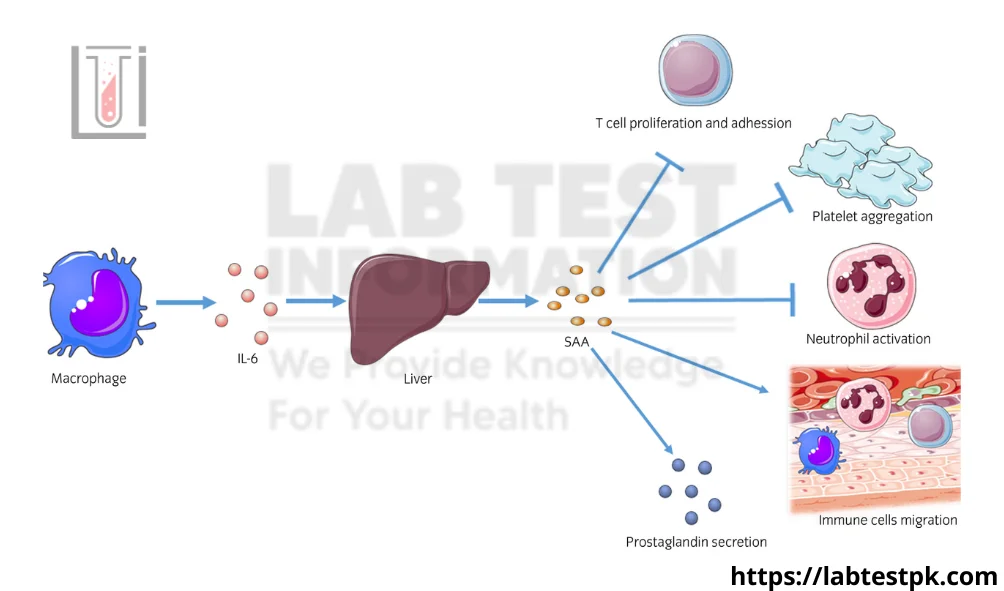
Serum Amyloid A (SAA) is a family of proteins that are synthesized in response to inflammation. These proteins are primarily produced by the liver and can be found in the bloodstream. SAA plays a role in the acute phase response of the immune system, which is the body’s rapid reaction to infection, injury, or other inflammatory processes.
There are two main isoforms of SAA, SAA1 and SAA2, and they are part of the acute-phase proteins, along with C-reactive protein (CRP) and fibrinogen. When the body experiences inflammation or infection, the levels of SAA in the blood can rise significantly.
SAA is often used as a biomarker in clinical medicine to assess the presence and extent of inflammation. Elevated SAA levels can be indicative of various conditions, including infectious diseases, autoimmune disorders, and chronic inflammatory conditions. It can be measured through blood tests and is particularly useful in monitoring disease activity and treatment response in conditions like rheumatoid arthritis, inflammatory bowel disease, and systemic infections.
In some cases, persistently elevated SAA levels can lead to the deposition of amyloid protein in tissues, a condition known as amyloidosis. Amyloidosis is a group of rare diseases characterized by the abnormal accumulation of amyloid proteins in various organs, which can lead to organ dysfunction.
Symptoms of Serum Amyloid A:
Serum Amyloid A (SAA) itself does not cause symptoms, as it is a protein produced by the liver in response to inflammation and tissue damage. However, elevated levels of SAA in the blood can be associated with underlying health conditions that cause various symptoms. The symptoms you experience would depend on the specific condition that is driving the increase in SAA. Some of the common symptoms associated with conditions related to elevated SAA levels include:
- Inflammation:
- Fever
- Fatigue
- Pain and swelling in affected joints or tissues
- Infections:
- Fever
- Chills
- Cough
- Fatigue
- Pain or discomfort in the area of the infection
- Autoimmune Diseases (e.g., rheumatoid arthritis, systemic lupus erythematosus):
- Joint pain and swelling
- Skin rashes
- Fatigue
- Muscle aches
- Cancer:
- Weight loss
- Fatigue
- Pain in the affected area (e.g., lung pain in lung cancer)
- Changes in appetite
- Cardiovascular Disease:
- Chest pain or angina
- Shortness of breath
- Fatigue
- Palpitations
- Chronic Kidney Disease:
- Swelling (edema), especially in the legs and ankles
- High blood pressure
- Changes in urination pattern
- Metabolic Syndromes (e.g., obesity, insulin resistance):
- Weight gain
- High blood pressure
- Elevated blood sugar levels
- Abnormal lipid profile
- Chronic Inflammatory Conditions (e.g., Crohn’s disease, ulcerative colitis, COPD):
- Abdominal pain and diarrhea (in inflammatory bowel diseases)
- Cough and shortness of breath (in COPD)
- Fatigue
How do healthcare providers diagnose AA amyloidosis?
Here are the steps healthcare providers may follow to diagnose AA amyloidosis:
- Clinical Evaluation: Healthcare providers will start by taking a detailed medical history and conducting a physical examination. They will inquire about symptoms, underlying conditions, and family history of amyloidosis. Symptoms may vary depending on which organs are affected, and they can include kidney dysfunction, gastrointestinal issues, heart problems, and others.
- Laboratory Tests: Various blood and urine tests are essential for diagnosing AA amyloidosis: a. Serum Amyloid A (SAA) Levels: Measuring the levels of SAA, a protein produced during inflammation, can indicate the presence of chronic inflammation and is often elevated in AA amyloidosis. b. Urinalysis: This can reveal signs of kidney dysfunction, such as proteinuria (the presence of excess proteins in the urine). c. Kidney Function Tests: Blood tests like creatinine and estimated glomerular filtration rate (eGFR) assess kidney function.d. Liver Function Tests: Liver function should be evaluated as the liver is a significant source of SAA.e. Complete Blood Count (CBC): Anemia or other blood abnormalities may be present in some cases.
- Tissue Biopsy: A definitive diagnosis of AA amyloidosis typically requires a tissue biopsy. The biopsy involves collecting a sample from an affected organ or tissue (commonly the kidney, liver, or gastrointestinal tract). This sample is examined under a microscope to confirm the presence of amyloid deposits. Special staining techniques, such as Congo red staining, can help identify amyloid deposits, which appear as characteristic apple-green birefringence under polarized light.
- Immunohistochemistry: Immunohistochemistry can be used to determine the specific type of amyloid protein present (in this case, AA amyloid), which helps in confirming the diagnosis.
- Imaging: Various imaging tests may be used to assess the extent of organ involvement and damage: a. X-rays: X-rays may be taken to examine bone and joint involvement. b. Echocardiogram: This ultrasound imaging of the heart can assess cardiac involvement in amyloidosis. c. Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): These imaging techniques can provide detailed images of organs affected by amyloid deposits.
- Genetic Testing: Genetic testing is usually not required to diagnose AA amyloidosis, as it is not a hereditary form of amyloidosis. However, it may be considered in cases where the diagnosis is uncertain or in the presence of a family history of amyloidosis.
Once a diagnosis of AA amyloidosis is confirmed, further testing and evaluation may be necessary to determine the underlying cause of chronic inflammation, such as an infectious or inflammatory condition.
Can I prevent AA amyloidosis?
Preventing AA amyloidosis largely involves managing the underlying conditions that can trigger abnormal protein deposition. Here are some steps to consider for prevention:
- Control Underlying Inflammatory Conditions: If you have an underlying inflammatory condition, such as rheumatoid arthritis or inflammatory bowel disease, work closely with your healthcare provider to manage and control the inflammation. This may involve medication, lifestyle changes, and regular follow-ups.
- Monitor and Treat Chronic Infections: Some chronic infections, such as tuberculosis, can trigger AA amyloidosis. If you have such infections, it is essential to seek appropriate treatment and follow your healthcare provider’s recommendations.
- Medication Management: Some medications, such as certain anti-inflammatory drugs, may be used to manage inflammation associated with chronic conditions. These medications should be taken under the supervision of a healthcare professional who can monitor their effects and adjust the treatment plan as needed.
- Lifestyle Modifications: In some cases, lifestyle modifications can help reduce the risk of AA amyloidosis. Maintaining a healthy diet, regular exercise, and a generally healthy lifestyle can contribute to overall well-being and potentially reduce inflammation in the body.
- Regular Check-ups: Regular medical check-ups can help identify underlying conditions and infections that might contribute to AA amyloidosis. Early diagnosis and management of these conditions can be crucial in preventing amyloidosis from developing.

[…] associated with autoimmune diseases, particularly systemic autoimmune diseases like systemic lupus erythematosus (SLE) and other connective tissue […]
[…] diseases: Conditions like systemic lupus erythematosus (SLE), rheumatoid arthritis, and Sjögren’s syndrome may be associated with […]
[…] was initially referred to as vitamin B13, it is not considered a true vitamin because the body can synthesize it. The term “vitamin B13” is no longer widely used in the context of essential […]
[…] Colitis: In some cases, the infection can lead to a condition called pseudomembranous colitis, characterized by the formation of inflammatory patches (pseudomembranes) on the colon […]
[…] Flow cytometryB. ELISAC. ImmunohistochemistryD. Southern […]
[…] Symptoms: Nausea, vomiting, and diarrhea can be associated with adrenal gland […]
[…] some cases, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to assess iron levels in the […]