Parkinson’s Disease symptoms
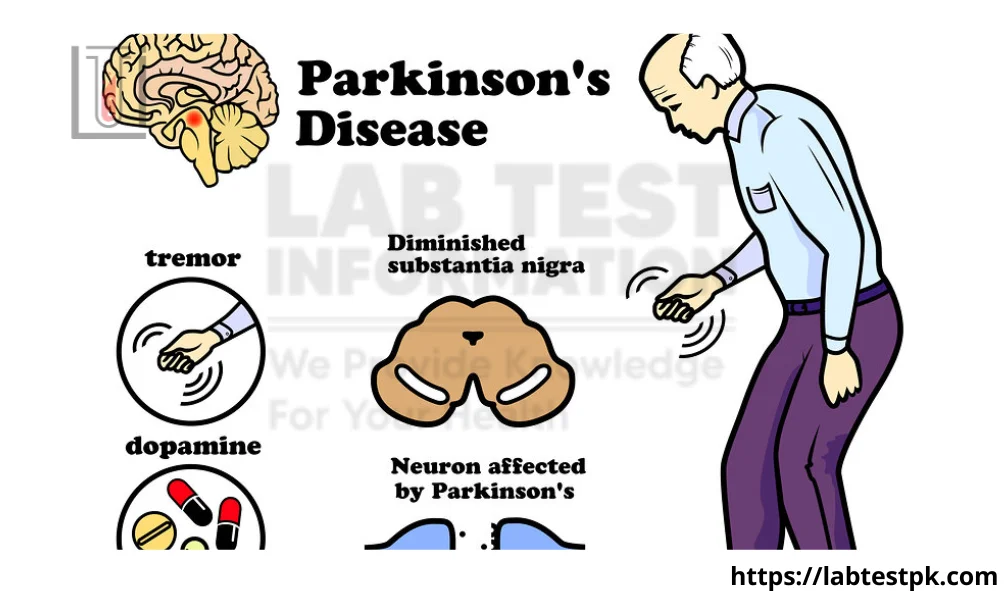
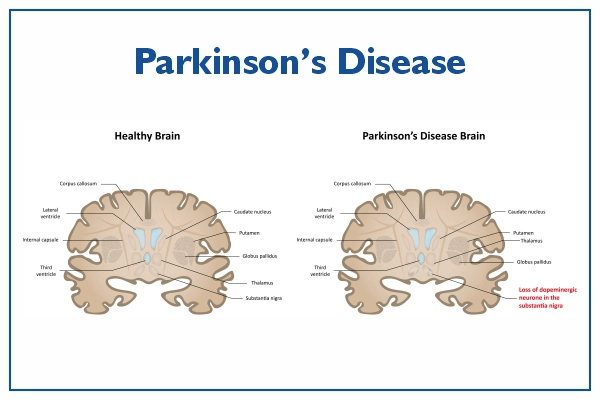
Parkinson’s Disease symptoms are a chronic progressive neurological disorder that disturbs muscle control, movement, and balance. It is characterized by muscle rigidity, tremor, and bradykinesia. It is a degenerative disease, that occurs due to degeneration of dopamine-producing cells in the substantia nigra, which results in dopamine deficiency. It most often develops in old age.
Types:
Parkinson’s disease is generally classified into two main types: idiopathic Parkinson’s disease (also known as primary or sporadic Parkinson’s disease) and secondary Parkinsonism. The vast majority of cases fall under idiopathic Parkinson’s disease. Here are brief descriptions of these types:
-
Idiopathic Parkinson’s Disease:
- Description: This is the most common form of Parkinson’s disease and accounts for the majority of cases. “Idiopathic” means that the cause is unknown.
- Characteristics: It is characterized by the gradual degeneration of dopamine-producing neurons in the substantia nigra, a region of the brain that plays a crucial role in movement control. The loss of dopamine leads to motor symptoms such as tremors, bradykinesia (slowness of movement), rigidity, and postural instability.
- Onset: Typically, idiopathic Parkinson’s disease is diagnosed in people over the age of 60, but it can occur earlier.
-
Secondary Parkinsonism:
- Description: Secondary Parkinsonism refers to Parkinsonian symptoms that are caused by factors other than the typical neurodegenerative processes seen in idiopathic Parkinson’s disease.
- Causes: It can be caused by various factors, including certain medications, head trauma, infections, and other neurological disorders. For example, some antipsychotic medications or drugs used to treat nausea may induce Parkinsonian symptoms.
- Characteristics: The symptoms of secondary Parkinsonism can closely resemble those of idiopathic Parkinson’s disease, but the underlying cause is different.
- Onset: The onset of symptoms in secondary Parkinsonism can be more abrupt than in idiopathic Parkinson’s disease.
Causes of Parkinson’s Disease
- Family History
- Genetic factors
- Viral infections
- Head trauma
- Antipsychotic drugs
- Environmental factors
Symptoms of Parkinson’s Disease
- Muscle rigidity
- Tremor
- Bradykinesia
- Posture problems
- Sleep disturbance
- Constipation
- Memory loss
- Swallowing difficulty
- Speech problems
- Male erectile dysfunction
Diagnostic Test for Parkinson’s Disease
- Family history
- Physical examination
- Neurological examination
- CT Scan and MRI
- CSF culture
Treatment of Parkinson’s Disease
1- Anti-Parkinson’s drugs
- Levodopa and carbidopa
2- Dopamine agonist
- Bromocriptine mesylate
3- Anticholinergic drugs
- Benztropine
4- Antiviral agents
5- Physical therapy
FAQs:
What is Parkinson’s disease?
- Parkinson’s disease is a progressive neurodegenerative disorder that affects movement. It occurs when nerve cells (neurons) in the brain that produce dopamine, a neurotransmitter important for movement control, become damaged or die.
2. What are the early symptoms of Parkinson’s disease?
- Early symptoms may include tremors, stiffness, slowness of movement, and difficulty with balance and coordination. Changes in handwriting (micrographia) and a reduced sense of smell can also be early indicators.
3. Is Parkinson’s disease hereditary?
- While most cases of Parkinson’s disease are sporadic, meaning they occur without a clear genetic link, some genetic factors can contribute to an increased risk. However, having a family history does not guarantee that an individual will develop the disease.
4. Can Parkinson’s disease be cured?
- There is currently no cure for Parkinson’s disease. Treatment focuses on managing symptoms, and various medications, physical therapy, and sometimes surgical interventions may be used to improve quality of life.
5. What causes Parkinson’s disease?
- The exact cause is not fully understood, but a combination of genetic and environmental factors is believed to contribute. Some cases are associated with specific genetic mutations, while others may be influenced by exposure to toxins or other environmental factors.
6. How is Parkinson’s disease diagnosed?
- Diagnosis is based on a clinical evaluation of symptoms, medical history, and sometimes specialized imaging studies. There is no definitive test for Parkinson’s disease, so the diagnosis is often made by a neurologist based on a thorough assessment.
7. Are there lifestyle changes that can help manage Parkinson’s symptoms?
- Yes, adopting a healthy lifestyle can be beneficial. Regular exercise, a balanced diet, and proper sleep are important. Physical and occupational therapy can also help manage symptoms and improve overall well-being.
8. Can Parkinson’s disease affect cognitive function?
- Yes, Parkinson’s disease can lead to cognitive changes over time. Some individuals may develop dementia in the later stages of the disease.
9. What is deep brain stimulation (DBS), and how is it used in Parkinson’s treatment?
- Deep brain stimulation is a surgical procedure where electrodes are implanted into specific areas of the brain to modulate abnormal neural activity. It can help alleviate motor symptoms in individuals with Parkinson’s disease who are not well controlled with medications alone.
10. Are there support services for individuals with Parkinson’s and their caregivers? – Yes, various support services, including support groups, counseling, and educational resources, are available for individuals with Parkinson’s and their caregivers. These services can provide assistance, information, and emotional support.


[…] The test results are reported as milligrams of albumin per gram of creatinine (mg/g). Normal values typically vary, but elevated levels of albumin in the urine may indicate kidney damage or dysfunction. […]
[…] is the name for a group of symptoms caused by disorders that affect the brain. It is not a specific disease. People with dementia may not be able to think well enough to do normal activities, such as getting […]
[…] Idiopathic ( exact cause is unknown ) […]
[…] successful treatment. This can be challenging to manage and may require additional interventionsParkinson’s Disease, such as fecal microbiota transplantation […]
[…] Celiac Disease […]