Orthopaedical tissue and fluid
Orthopaedical tissue and fluid are integral components of the musculoskeletal system and play crucial roles in maintaining the structure and function of bones, joints, ligaments, tendons, and other related structures. Here’s an overview of some key orthopedic tissues and fluids:
Orthopedic Tissues:
-
Bone:
- Structure: Bones provide structural support to the body, protect vital organs, and serve as sites for muscle attachment.
- Function: They contribute to body movement, mineral storage (calcium and phosphorus), and blood cell formation (in the bone marrow).
- Joint Tissues:
- Articular Cartilage: A smooth, elastic tissue covering the ends of bones in joints. It helps reduce friction and absorb shock during joint movement.
- Synovium: A thin membrane that lines joint cavities and produces synovial fluid.
- Ligaments:
- Function: Connect bone to bone, providing stability to joints.
- Tendons:
- Function: Connect muscle to bone, transmitting the force generated by muscles to the bone for movement.
- Muscles:
- Function: Muscles contract and relax to facilitate movement and provide support to joints.
- Connective Tissues:
- Fascia: Connective tissue that surrounds muscles, groups of muscles, blood vessels, and nerves.
- Periosteum: A dense layer of vascular connective tissue covering the bones.
Orthopedic Fluids:
- Synovial Fluid:
- Location: Found in joint cavities.
- Function: Lubricates joints, nourishes articular cartilage, and reduces friction during movement.
- Cerebrospinal Fluid (CSF):
- Location: Surrounds the brain and spinal cord.
- Function: Provides buoyancy and protection to the central nervous system.
- Blood:
- Function: Supplies oxygen, nutrients, and immune cells to orthopedic tissues.
Orthopedic Disorders and Diseases:
- Osteoarthritis:
- Involves: Degeneration of articular cartilage in joints.
- Rheumatoid Arthritis:
- Involves: Inflammation of the synovium, leading to joint damage.
- Fractures:
- Involves: Breaks or cracks in bones.
- Tendonitis:
- Involves: Inflammation of tendons.
- Ligament Injuries:
- Involves: Sprains or tears in ligaments.
Understanding the anatomy, function, and pathology of these orthopedic tissues and fluids is essential for medical professionals involved in orthopedic care, including orthopedic surgeons, rheumatologists, and physical therapists.
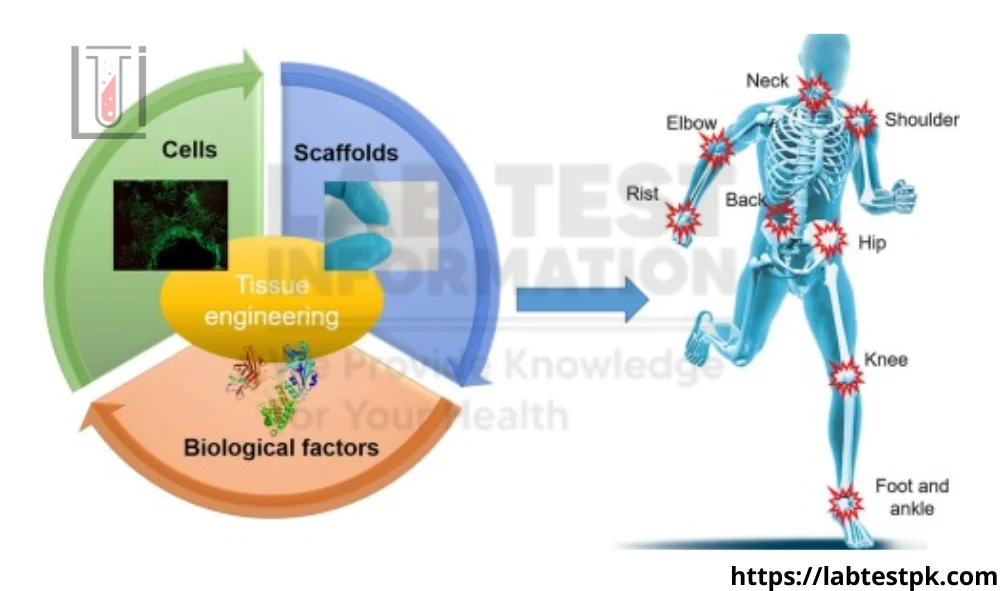
Stem Cells, Differentiation, and Osteogenesis:
Stem cells, differentiation, and osteogenesis are interconnected concepts in the field of biology, particularly in the study of developmental biology and regenerative medicine. Let’s break down each of these concepts:
-
Stem Cells:
- Stem cells are undifferentiated cells with the unique ability to develop into various specialized cell types.
- They are characterized by two key properties: self-renewal (the ability to divide and produce identical stem cells) and pluripotency or multipotency (the ability to differentiate into multiple cell types).
- There are two main types of stem cells: embryonic stem cells, which are derived from embryos, and adult or somatic stem cells, which are found in various tissues throughout the body.
-
Differentiation:
- Differentiation is the process by which a less specialized cell becomes more specialized, acquiring specific functions and characteristics.
- As stem cells undergo differentiation, they become committed to a particular cell lineage and gradually acquire the structural and functional features of that specific cell type.
- The process of differentiation involves changes in gene expression, cellular morphology, and function.
-
Osteogenesis:
- Osteogenesis specifically refers to the process of bone formation.
- During osteogenesis, mesenchymal stem cells (a type of adult stem cell) differentiate into osteoblasts, which are the cells responsible for synthesizing the bone matrix and promoting mineralization.
- Osteoblasts play a crucial role in the development and maintenance of bone tissue. They produce and secrete the extracellular matrix of bone, which includes collagen and various minerals such as calcium and phosphate.
- As the bone matrix is mineralized, osteoblasts may become surrounded by the mineralized matrix and transform into osteocytes, the mature bone cells that are embedded within the bone tissue.
In summary, stem cells serve as the source for various cell types in the body through the process of differentiation. Osteogenesis is a specific example of differentiation where mesenchymal stem cells give rise to osteoblasts, leading to the formation and maintenance of bone tissue. Understanding these processes is critical for both developmental biology and applications in regenerative medicine, where the manipulation of stem cells and their differentiation pathways holds promise for treating various diseases and injuries, including those related to bone and musculoskeletal tissues.
Bone, the Fundamental Orthopaedic Tissue Cellular Biology:
The cellular biology of bone involves several key cell types and processes that contribute to its development, maintenance, and repair.
Key Cell Types in Bone Tissue:
-
Osteoblasts:
- Function: Osteoblasts are responsible for bone formation. They produce and secrete the organic components of the bone matrix, including collagen and other proteins.
- Activity: Osteoblasts play a crucial role in the mineralization of bone by depositing hydroxyapatite crystals onto the matrix.
- Osteocytes:
- Function: Osteocytes are mature osteoblasts that have become embedded in the bone matrix. They maintain the bone tissue and regulate mineral homeostasis.
- Activity: Osteocytes communicate with each other and with other bone cells through a network of cellular processes within tiny channels called canaliculi.
- Osteoclasts:
- Function: Osteoclasts are responsible for bone resorption, breaking down bone tissue to release minerals into the bloodstream.
- Activity: Osteoclasts secrete enzymes and acids that dissolve the mineralized matrix, and they play a crucial role in bone remodeling and maintenance.
Bone Matrix:
- Organic Matrix:
- Composition: The organic matrix of bone is primarily composed of collagen fibers, which provide flexibility and tensile strength to the bone.
- Role: It forms a framework for mineral deposition and contributes to the overall structure of the bone.
- Inorganic Matrix:
- Composition: The inorganic matrix consists mainly of hydroxyapatite crystals, which are composed of calcium and phosphate.
- Role: Provides rigidity and hardness to the bone, contributing to its compressive strength.
Bone Development and Remodeling:
- Ossification:
- Intramembranous Ossification: Formation of flat bones directly from mesenchymal cells.
- Endochondral Ossification: Formation of long bones through the replacement of cartilage by bone tissue.
- Bone Remodeling:
- Continuous Process: Bone tissue undergoes constant remodeling throughout life to adapt to mechanical stresses, repair microdamage, and maintain mineral balance.
- Balanced Activity: Osteoclasts and osteoblasts work in concert to maintain the integrity and strength of the bone.
FAQs:
- What is synovial fluid?
- Answer: Synovial fluid is a viscous fluid found in joints, providing lubrication and nourishment to the articular cartilage. It also helps reduce friction between joint surfaces during movement.
- What is the function of articular cartilage?
- Answer: Articular cartilage covers the ends of bones in joints and serves as a cushion, reducing friction and facilitating smooth joint movement.
- What are the common causes of joint pain?
- Answer: Joint pain can result from various causes, including osteoarthritis, rheumatoid arthritis, injuries, inflammation, and infectious diseases affecting the joints.
- What is osteoarthritis?
- Answer: Osteoarthritis is a degenerative joint disease characterized by the breakdown of joint cartilage and the underlying bone, leading to pain, stiffness, and reduced joint mobility.
- How are fractures treated in orthopedics?
- Answer: Fractures are typically treated by immobilizing the affected area using casts, splints, or braces. Severe fractures may require surgical intervention, such as the insertion of metal plates or screws.
- What is a torn ligament, and how is it treated?
- Answer: A torn ligament is a stretch or tear in the tough bands of tissue connecting bones to each other. Treatment may involve rest, physical therapy, and in some cases, surgical repair.
- How does physical therapy benefit orthopedic conditions?
- Answer: Physical therapy helps improve strength, flexibility, and range of motion. It can be beneficial in the rehabilitation of orthopedic conditions, such as joint injuries or after orthopedic surgery.
- What are tendons, and what is their function?
- Answer: Tendons are fibrous tissues that connect muscles to bones. They transmit the force generated by muscles to the bones, allowing movement of the joints.
- What is a common orthopedic surgical procedure?
- Answer: Total joint replacement, such as hip or knee replacement, is a common orthopedic surgical procedure. It involves replacing a damaged joint with a prosthetic implant.
- How is inflammation in joints managed?
- Answer: Inflammation in joints is often managed with nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, physical therapy, and lifestyle modifications.


Good work
[…] is the loss of mental functions such as thinking, memory, and reasoning this is severe enough to interfere with a person’s […]
[…] Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness in the voluntary skeletal muscles, which are your body’s muscles for movement. It mostly affected muscles eyes, face, […]
[…] by muscle rigidity, tremor, and bradykinesia. It is a degenerative disease, that occurs due to degeneration of dopamine-producing cells in the substantia nigra, which results in dopamine deficiency. It most […]
[…] containing ingredients like benzoyl peroxide, salicylic acid, or alpha hydroxy acids can help unclog pores and reduce […]