Lupus anticoagulant (LA) is an autoimmune disorder in which the immune system mistakenly produces antibodies that target certain proteins involved in blood clotting. Despite its name, lupus anticoagulant does not cause bleeding; instead, it predisposes individuals to excessive blood clot formation. This condition is associated with an increased risk of abnormal blood clotting, which can lead to conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), and other thrombotic events.
Here are some key points about lupus anticoagulants:
-
Antibodies:
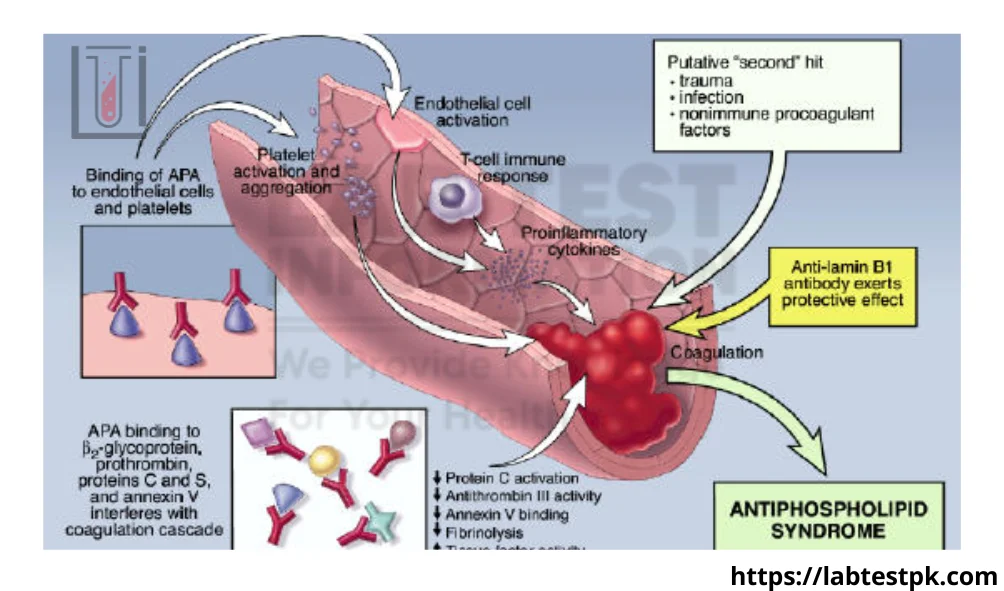
In lupus anticoagulants, the immune system produces antibodies that target phospholipids. These antibodies are known as antiphospholipid antibodies. -
Clotting Abnormalities:
Despite its name, lupus anticoagulant doesn’t function as an anticoagulant (blood thinner). Instead, it interferes with the normal clotting process, leading to an increased risk of abnormal blood clot formation. -
Association with Systemic Lupus Erythematosus (SLE):
Lupus anticoagulant is often associated with systemic lupus erythematosus, an autoimmune disease that can affect various organs and tissues in the body. -
Clinical Manifestations:
Individuals with lupus anticoagulants may experience recurrent blood clotting events, particularly in veins and arteries. This can lead to serious health issues, such as strokes, heart attacks, and pregnancy complications. -
Diagnosis:
The diagnosis of lupus anticoagulant involves specialized blood tests to detect the presence of antiphospholipid antibodies and assess their impact on blood clotting. It’s important to note that the name “lupus anticoagulant” can be confusing, as it does not reflect the actual anticoagulant properties of this condition. -
Treatment:
Treatment may involve anticoagulant medications to prevent the formation of blood clots. In some cases, individuals may also receive immunosuppressive therapy to manage the autoimmune component of the condition. -
Monitoring and Prevention:
Regular monitoring of blood clotting parameters is important for individuals with lupus anticoagulants. Prevention measures, such as the use of anticoagulant medications, may be recommended, especially in situations where there is a higher risk of clot formation.
What are lupus anticoagulants and anticardiolipin antibodies?
Lupus anticoagulants (LAs) and anticardiolipin antibodies (aCL) are both associated with autoimmune disorders, particularly systemic lupus erythematosus (SLE), but they can also be found in individuals without autoimmune diseases. These antibodies are known for their role in causing abnormal blood clotting, which can lead to various health issues.
-
Lupus Anticoagulants (LAs):
-
Nature:
Lupus anticoagulants are not anticoagulants in the traditional sense; rather, they are a type of autoantibody. -
Function:
Despite the name, LAs promote rather than inhibit blood clotting. They interfere with the normal clotting process and increase the risk of abnormal clot formation. -
Associated Conditions:
LAs are frequently associated with systemic autoimmune diseases such as systemic lupus erythematosus (SLE) but can also be found in individuals without an apparent autoimmune disorder. -
Clinical Significance:
The presence of lupus anticoagulants is associated with an increased risk of thrombosis (abnormal blood clotting) and pregnancy complications.
-
-
Anticardiolipin Antibodies (aCL):
-
Nature:
Anticardiolipin antibodies are also autoantibodies that target cardiolipin, a phospholipid found in cell membranes. -
Function:
Similar to lupus anticoagulants, anticardiolipin antibodies can interfere with the blood clotting process and may contribute to abnormal clot formation. - Associated Conditions: Anticardiolipin antibodies are often found in individuals with autoimmune diseases, particularly systemic lupus erythematosus (SLE), but they can also be present in those without apparent autoimmune conditions.
- Clinical Significance: The presence of anticardiolipin antibodies is associated with an increased risk of thrombosis and can also lead to pregnancy complications, such as recurrent miscarriages.
-
Both lupus anticoagulants and anticardiolipin antibodies are tested as part of the antiphospholipid antibody (APLA) panel, which also includes tests for anti-beta-2 glycoprotein I antibodies. The presence of these antibodies, especially when detected in the context of clinical symptoms or a history of blood clotting events, can influence medical management, such as the use of anticoagulant medications to reduce the risk of thrombosis.
What are the symptoms of lupus anticoagulant syndrome?
The symptoms of lupus anticoagulant syndrome can vary, and some individuals may not experience any symptoms. When symptoms do occur, they can include:
- Blood Clots: This is the hallmark of lupus anticoagulant syndrome. Blood clots can form in veins (venous thrombosis) or arteries (arterial thrombosis). This can lead to conditions such as deep vein thrombosis (DVT), pulmonary embolism, stroke, or heart attack.
- Recurrent Miscarriages: Women with lupus anticoagulant syndrome may be at an increased risk of recurrent miscarriages and pregnancy complications.
- Skin Symptoms: Some individuals may develop skin symptoms, such as livedo reticularis, which is a mottled, purplish discoloration of the skin.
- Neurological Symptoms: Lupus anticoagulant syndrome can cause neurological symptoms, including headaches, seizures, and cognitive impairment.
- Raynaud’s Phenomenon: This is a condition where certain parts of the body, usually fingers and toes, turn white or blue in response to cold or stress.
- Joint Pain: Some people with lupus anticoagulant syndrome may experience joint pain and inflammation.
- Heart Valve Abnormalities: In rare cases, the syndrome can lead to heart valve abnormalities.

[…] are used in the diagnosis and management of various conditions, including bleeding disorders and clotting disorders. Abnormal platelet aggregation can be indicative of platelet function disorders, which […]
Is Lupus Coagulant contagious around people. I have it .
[…] Test, Tacrolimus is a medication that is commonly used as an immunosuppressive drug. It is often prescribed to prevent rejection in organ transplant recipients and to treat […]
[…] that not everyone with HFE gene mutations develops hemochromatosis, and other factors can also influence the condition. Regular monitoring and management, if needed, can help individuals with […]
[…] diseases: Conditions like rheumatoid arthritis, lupus, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), and psoriasis cause the […]
[…] healthcare professional collects a sample of pus from the infected area using a sterile swab or […]
[…] is often done through blood tests. Detecting these antibodies can help in the diagnosis of autoimmune liver diseases, especially PBC. However, it’s important to note that the presence of […]
[…] you are taking any blood-thinning medicines (anticoagulants), including Aspirin, warfarin, […]
[…] Willebrand factor is a large glycoprotein that plays a crucial role in blood clotting by assisting platelets in adhering to the site of blood […]
Is Lupus Coagulant contagious to people around me. I have it.
Is Lupus Coagulant contAGIOUS TO PEOPLE AROUND ME ? i HAVE IT.