Insulin Response Blood Test, 3-Specimens
Insulin Response Blood Test, An insulin response blood test, also known as an insulin tolerance test (ITT) or a glucose tolerance test (GTT), is a medical diagnostic test that measures how well your body regulates blood sugar levels and responds to insulin. It is primarily used to diagnose conditions like diabetes and hypoglycemia.
Here’s how the test is typically conducted:
- Fasting: You will be asked to fast for a certain period, usually overnight. This means no food or drink (except water) for 8-12 hours before the test.
- Baseline Measurements: When you arrive at the healthcare facility, a healthcare professional will measure your fasting blood sugar level and, in some cases, your fasting insulin level.
- Glucose Solution: You will be asked to drink a specific amount of glucose solution, usually a high-concentration sugar solution. The glucose solution is sweet and may not be very pleasant to taste.
- Monitoring: Over the next few hours (usually 2-3 hours), blood samples will be taken at regular intervals (usually every 30 minutes) to measure your blood sugar levels.
- Insulin Level: In some cases, your insulin levels may be measured at various points during the test.
The results of the insulin response blood test can help diagnose various conditions:
- Diabetes: If your blood sugar levels remain elevated after drinking the glucose solution, it may indicate diabetes. Your blood sugar response pattern can help determine whether you have type 1 or type 2 diabetes.
- Hypoglycemia: In some cases, the test can help diagnose reactive hypoglycemia, a condition where blood sugar levels drop too low after consuming high-sugar meals.
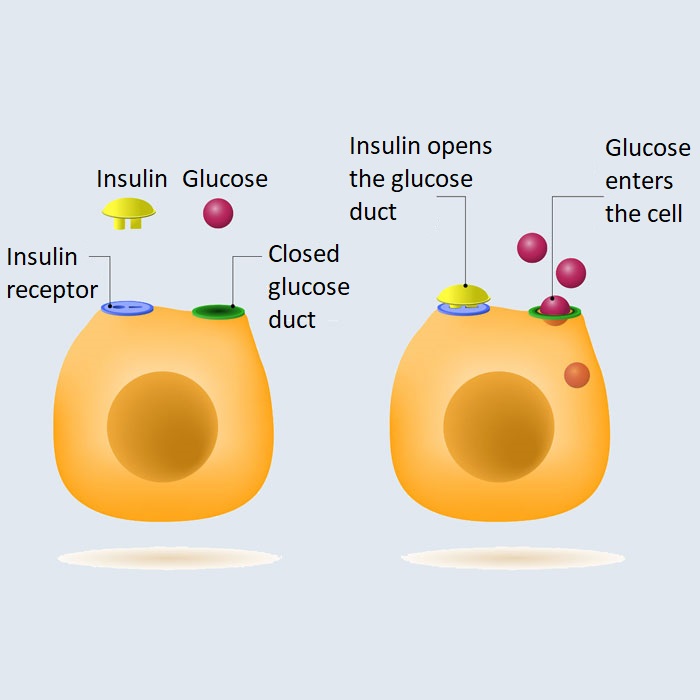
- Insulin Resistance: Measuring insulin levels can help determine if you have insulin resistance, a condition in which the body’s cells don’t respond properly to insulin, which can lead to type 2 diabetes.
What causes elevated insulin levels?
Elevated insulin levels, known as hyperinsulinemia, can be caused by a variety of factors and conditions. Insulin is a hormone produced by the pancreas that plays a key role in regulating blood sugar levels and facilitating the uptake of glucose into cells. When insulin levels are consistently high, it can indicate an underlying health issue. Some common causes of elevated insulin levels include:
- Insulin Resistance: This is a condition in which the body’s cells do not respond effectively to insulin, so the pancreas produces more insulin to compensate. It is a hallmark of type 2 diabetes and is often associated with obesity.
- Type 2 Diabetes: People with type 2 diabetes often have elevated insulin levels because their bodies do not use insulin efficiently to regulate blood sugar.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder in women that can lead to insulin resistance, causing elevated insulin levels. This can result in high blood sugar levels and an increased risk of diabetes.
- Excessive Carbohydrate Intake: Consuming large quantities of carbohydrates, especially refined and sugary ones, can cause a spike in blood sugar, leading to increased insulin production. Over time, this can contribute to insulin resistance.
- Obesity: Excess body fat, especially abdominal fat, is strongly associated with insulin resistance and elevated insulin levels. Losing weight and maintaining a healthy body weight can improve insulin sensitivity.
- Certain Medications: Some medications, such as corticosteroids and antipsychotic drugs, can lead to elevated insulin levels as a side effect.
- Chronic Stress: Stress can lead to the release of stress hormones like cortisol, which can affect insulin sensitivity. Chronic stress can contribute to insulin resistance and elevated insulin levels.
- Certain Medical Conditions: Some medical conditions, like acromegaly (excess growth hormone) and Cushing’s syndrome (excess cortisol), can lead to elevated insulin levels as a secondary effect.
- Gestational Diabetes: During pregnancy, some women develop gestational diabetes, which leads to elevated insulin levels. This typically resolves after childbirth.
- Genetics: Some individuals may have a genetic predisposition to insulin resistance and higher insulin levels.
What causes insulin resistance?
Insulin resistance is a condition in which the body’s cells do not respond effectively to the hormone insulin. This can lead to elevated blood sugar levels and, over time, can contribute to the development of type 2 diabetes. Several factors can contribute to the development of insulin resistance:
- Genetics: Some people may have a genetic predisposition to insulin resistance. If you have a family history of diabetes or insulin resistance, you may be at a higher risk.
- Obesity: Excess fat, particularly abdominal or visceral fat, is strongly associated with insulin resistance. Adipose (fat) tissue can release chemicals and hormones that interfere with insulin’s actions.
- Sedentary Lifestyle: Lack of physical activity and exercise can contribute to obesity and insulin resistance. Regular exercise helps improve insulin sensitivity.
- Poor Diet: Diets high in sugar, refined carbohydrates, and saturated fats can contribute to insulin resistance. Consuming large amounts of processed foods and sugary beverages can be particularly detrimental.
- Inflammation: Chronic low-level inflammation in the body can impair insulin sensitivity. Inflammatory chemicals can interfere with insulin signaling.
- Hormonal Imbalances: Conditions like polycystic ovary syndrome (PCOS) can lead to hormonal imbalances that contribute to insulin resistance.
- Sleep Problems: Inadequate or poor-quality sleep can disrupt the body’s hormonal balance and lead to insulin resistance.
- Stress: Chronic stress can elevate stress hormones like cortisol, which can lead to insulin resistance.
- Aging: As people age, they may become more insulin resistant, although this is not inevitable.
- Medications: Certain medications, such as corticosteroids and antipsychotic drugs, can induce insulin resistance as a side effect.
- Smoking: Smoking is associated with an increased risk of insulin resistance and type 2 diabetes.
- Gestational Diabetes: Women who develop gestational diabetes during pregnancy may be at higher risk of insulin resistance in the future.
It’s important to note that these factors often interact with one another, and the development of insulin resistance is a complex process. Managing and preventing insulin resistance typically involves lifestyle modifications such as maintaining a healthy weight, eating a balanced diet, staying physically active, managing stress, and getting adequate sleep. In some cases, medication or insulin therapy may be necessary to manage insulin resistance and diabetes.
When should I order an Insulin Response Blood Test, 3-Specimens?
Here are some general considerations:
- Diagnosis of Diabetes: If your healthcare provider suspects that you may have diabetes or prediabetes, they may order an insulin response test as part of the diagnostic process. The timing of the test will be determined by your provider based on your medical history and symptoms.
- Glucose Tolerance Test: An oral glucose tolerance test (OGTT) is a common test that involves fasting overnight and then drinking a glucose solution. Blood samples are taken at specific intervals, usually at baseline (fasting), 1 hour, 2 hours, and sometimes 3 hours after consuming the glucose solution. This test can help diagnose gestational diabetes, type 2 diabetes, or impaired glucose tolerance.
- Insulin Resistance Assessment: If your healthcare provider suspects insulin resistance, they may order a 3-specimen insulin response test to assess how your body releases insulin in response to glucose. The timing for this test will depend on your specific circumstances.
- Monitoring: If you already have diabetes or another condition that affects insulin regulation, your healthcare provider may order periodic insulin response tests to monitor how your treatment plan is working.
Your healthcare provider will determine the specific timing for these tests based on your health situation. It’s important to follow your healthcare provider’s instructions regarding fasting, any medication adjustments, and other preparations required for the test.


:max_bytes(150000):strip_icc()/how-do-i-know-if-i-have-insulin-resistance-2616646-v2-5c455306c9e77c0001db3ac7.png)
[…] muscle and others are damaged. when the total CPK level is elevated, it usually indicates injury or stress to heart muscle, skeletal muscle, or injury to the […]
[…] diet: Diets high in processed foods, sugar, and unhealthy fats, and low in fruits, vegetables, and whole grains can […]
[…] you have Type 1 diabetes with positive autoantibodies. In that case, you are likely to require insulin therapy from the outset, whereas Type 2 diabetes may initially be managed with lifestyle […]
[…] sample for the presence of the parasite’s cysts or trophozoites. Sometimes, serologic tests (blood tests) are also used to detect antibodies against the […]
[…] type of diabetes that develops during pregnancy. It occurs when the body can’t produce enough insulin to meet the increased needs of pregnancy. This condition can lead to high blood sugar levels, which […]
[…] hemoglobin, the protein in red blood cells that carries oxygen. The abnormal hemoglobin causes red blood cells to become rigid and shaped like sickles, leading to various complications such as pain, anemia, and […]
[…] the immune system mistakenly attacks and damages the adrenal glands, leading to a deficiency in the hormones they produce. The primary hormone deficiency in Addison’s disease is cortisol, but it can […]