Histoplasma (Histoplasmosis)
Histoplasma is a genus of dimorphic fungi that includes several species, with Histoplasma capsulatum being the most clinically significant. These fungi are responsible for causing a disease known as histoplasmosis. Histoplasmosis is a fungal infection that primarily affects the lungs but can also involve other organs in the body.
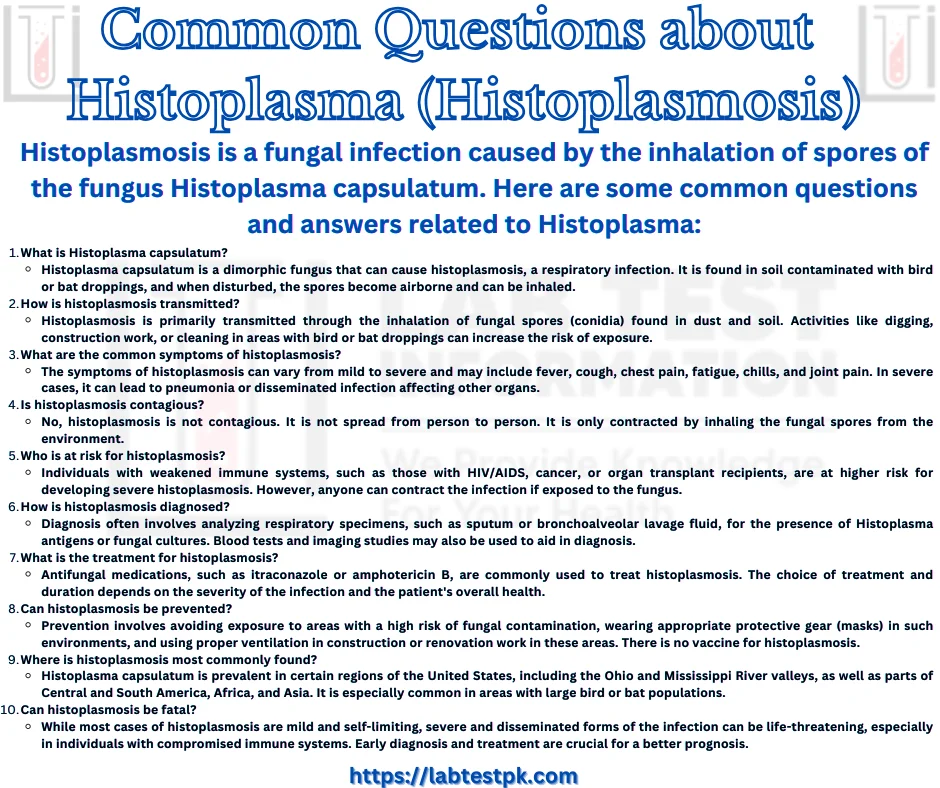
Here are some key points about Histoplasma and histoplasmosis:
- Fungal Pathogen: Histoplasma capsulatum is the primary species of Histoplasma that causes human infections. It is found in soil, particularly in areas with bird or bat droppings, as the fungus grows in nitrogen-rich environments. When the soil is disturbed, such as during construction or excavation, the fungal spores can become airborne and be inhaled by humans, leading to infection.
- Dimorphic Fungus: Histoplasma capsulatum is a dimorphic fungus, which means it has two different growth forms: a mold form and a yeast form. In the environment (soil), it exists as a mold with filamentous structures. However, when it infects a host (human or animal), it converts to a yeast form, which is the pathogenic form.
- Histoplasmosis: Histoplasmosis is the disease caused by Histoplasma infection. The severity of the disease can range from mild or asymptomatic to severe and life-threatening, depending on the individual’s immune system and the amount of exposure to the fungus. Common symptoms of histoplasmosis include fever, cough, chest pain, and fatigue. In severe cases, it can lead to pneumonia and other complications.
- Geographic Distribution: Histoplasma capsulatum is found in various regions around the world, but it is particularly common in certain parts of North and Central America, including the Ohio and Mississippi River valleys in the United States. The fungus thrives in soil enriched with bird and bat droppings.
Signs and Symptoms of Histoplasma:
Histoplasmosis is a fungal infection caused by the inhalation of spores from the fungus Histoplasma capsulatum. The severity and presentation of histoplasmosis can vary widely, and in many cases, it may not cause any symptoms (asymptomatic infection). When symptoms do occur, they can resemble those of other respiratory illnesses. Here are some common signs and symptoms of histoplasmosis:
- Flu-like Symptoms: Many cases of histoplasmosis start with symptoms similar to the flu, including fever, chills, headache, muscle aches, and fatigue.
- Respiratory Symptoms: As the infection progresses, it can affect the respiratory system, leading to symptoms such as a dry cough, chest pain, and shortness of breath.
- Fever: Histoplasmosis can cause a persistent fever that may come and go.
- Chest Pain: Some individuals with histoplasmosis experience chest pain, especially if the infection leads to lung inflammation.
- Cough: A productive or dry cough can develop as the infection affects the lungs.
- Weight Loss: Unintentional weight loss is a possible symptom, particularly in severe cases of histoplasmosis.
- Enlarged Lymph Nodes: Swollen lymph nodes, especially in the neck and armpits, can be a sign of disseminated histoplasmosis, a more severe form of the infection.
- Joint Pain: Joint pain (arthralgia) is occasionally reported in individuals with histoplasmosis.
- Oral Ulcers: Some people may develop mouth ulcers as a result of histoplasmosis.
- Skin Rashes: Skin rashes or lesions can occur, particularly in cases of disseminated histoplasmosis.
It’s important to note that the severity and presentation of histoplasmosis can vary depending on factors such as the individual’s overall health and immune system status. In some cases, the infection can become chronic and lead to long-term lung problems. Disseminated histoplasmosis, which occurs when the fungus spreads to other organs beyond the lungs, is more severe and can be life-threatening, especially in people with weakened immune systems.
Risk and Prevention:
Here are some key points regarding the risk and prevention of histoplasmosis:
Risk Factors:
- Location: Histoplasmosis is most prevalent in certain geographic regions, primarily in the United States, Central and South America, and parts of Africa and Asia. The risk of exposure is higher in areas where the fungus is endemic.
- Occupational Exposure: Certain occupations, such as cave explorers, construction workers, and agricultural workers, are at higher risk of exposure to Histoplasma spores because they may disturb soil or bird and bat droppings where the fungus can be found.
- Environmental Exposure: Spending time in environments where the fungus is present, such as caves, old buildings, or bird roosts, can increase the risk of infection.
- Immunocompromised Individuals: People with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy, are at higher risk of developing severe forms of histoplasmosis if they become infected.
Prevention:
- Protective Clothing: If you are in an area where Histoplasma is likely to be present, wear protective clothing, such as gloves and a mask, to reduce the risk of inhaling spores or coming into contact with contaminated soil or bird droppings.
- Limit Exposure: Avoid activities that involve disturbing soil or bird and bat droppings in endemic areas. If you need to perform such activities, take precautions and use proper respiratory protection.
- Travel Precautions: Travelers to endemic regions should be aware of the risk and take precautions to minimize exposure. This includes staying away from caves or areas with accumulations of bird or bat droppings.
- Infection Control for Healthcare Workers: Healthcare workers should be aware of the risk of histoplasmosis when treating patients with the infection, particularly those with weakened immune systems. Standard infection control measures should be followed.
- Antifungal Medications: In some cases, individuals at high risk of severe histoplasmosis, such as those with compromised immune systems, may be prescribed antifungal medications as a preventive measure. This is typically done under the guidance of a healthcare professional.
- Public Health Measures: In regions where histoplasmosis is endemic, public health measures may be implemented to reduce the risk of exposure. This can include cleaning up areas with large accumulations of bird or bat droppings.
It’s essential to be aware of the risk factors and take appropriate precautions, especially if you live in or plan to visit areas where Histoplasma is endemic or if you have a weakened immune system.
Diagnosis and testing:
Histoplasma is a type of fungus that can cause a disease called histoplasmosis when it infects humans. Diagnosing histoplasmosis typically involves a combination of clinical evaluation, medical history, and laboratory tests. Here are the common methods used for diagnosing and testing for Histoplasma infection:
- Clinical Evaluation:
- Symptoms: The doctor will assess your symptoms, which can vary depending on the severity of the infection but may include fever, cough, chest pain, fatigue, and more.
- Medical History: Your doctor will inquire about your travel history to endemic areas (regions where Histoplasma is commonly found) and any other risk factors for exposure to the fungus.
- Radiological Imaging:
- Chest X-rays or CT scans may be performed to evaluate the extent of lung involvement. This can help identify characteristic findings such as pulmonary nodules or infiltrates.
- Laboratory Tests:
- Histopathology: Examination of tissue samples (biopsy) under a microscope can reveal the presence of Histoplasma yeast cells or granulomas in affected tissues. This is especially important when there are skin or organ lesions.
- Microscopy: Sputum or other respiratory samples can be examined under a microscope to detect the presence of Histoplasma organisms. Staining techniques like Gomori methenamine silver (GMS) or periodic acid-Schiff (PAS) may be used to highlight the fungus.
- Cultures: Fungal cultures can be performed on various clinical specimens, such as blood, bone marrow, or respiratory samples, to isolate and identify Histoplasma species.
- Serology: Blood tests can be conducted to detect specific antibodies (IgG and IgM) against Histoplasma antigens. Serologic tests include enzyme immunoassays (EIA) and complement fixation tests. Rising antibody titers over time may indicate an active infection.
- Molecular Testing:
- Polymerase chain reaction (PCR) can be used to detect Histoplasma DNA in clinical samples. This method is highly sensitive and specific but may not be widely available.
- Antigen Testing:
- A urinary antigen test is available for the detection of Histoplasma antigen in the urine. This test is particularly useful in diagnosing disseminated histoplasmosis and is less invasive than some other methods.
- Blood Tests:
- Complete blood count (CBC) and blood chemistry tests may be conducted to assess overall health and check for abnormalities related to Histoplasma infection, such as anemia or liver function abnormalities.
The choice of diagnostic tests depends on the patient’s clinical presentation, risk factors, and the suspected form of histoplasmosis (acute pulmonary, chronic pulmonary, or disseminated).
Treatment of Histoplasma:
The treatment of histoplasmosis depends on the severity of the infection, the patient’s overall health, and the presence of any underlying medical conditions. Here are the common treatment approaches:
- Observation (Mild Cases): In some cases, especially if the infection is mild and the patient has a healthy immune system, treatment may not be necessary. The body’s immune system can often control the infection on its own. However, monitoring the patient’s condition is essential.
- Antifungal Medications: If the infection is moderate to severe or if the patient has a weakened immune system (e.g., due to HIV/AIDS, organ transplant, or chemotherapy), antifungal medications are typically prescribed. The most commonly used antifungal drugs for histoplasmosis include:
- Itraconazole: This is often the first choice for treating histoplasmosis. It’s usually taken orally and is effective for both acute and chronic forms of the disease.
- Amphotericin B: This medication is more potent but is usually reserved for severe or disseminated cases of histoplasmosis. It can be given intravenously.
- Fluconazole: In some cases, fluconazole may be used, especially for maintenance therapy or if itraconazole is not well-tolerated.
- Duration of Treatment: The duration of treatment can vary depending on the form and severity of histoplasmosis. Acute pulmonary histoplasmosis is typically treated for 6-12 weeks, while chronic pulmonary or disseminated histoplasmosis may require longer courses of treatment, often lasting several months.
- Management of Complications: If histoplasmosis leads to complications such as respiratory distress, organ failure, or severe systemic symptoms, additional supportive care and interventions may be necessary. This can include oxygen therapy, mechanical ventilation, or treatment for specific organ involvement.
- Prevention: Prevention is crucial, especially for individuals at higher risk of histoplasmosis. This may involve avoiding activities that disturb soil and bird or bat droppings, wearing protective gear when working in these environments and taking antifungal prophylaxis for individuals with compromised immune systems.
It’s essential for individuals with histoplasmosis to follow their healthcare provider’s recommendations and complete the full course of antifungal treatment to ensure the infection is completely eradicated. Regular follow-up visits and monitoring are also important to assess treatment response and address any potential side effects of antifungal medications.


[…] they work: Various drug testing methods include immunoassays and chromatography. Immunoassays are rapid and less expensive, providing initial results, while confirmatory tests like gas […]
[…] is a genus of dimorphic fungi, and the most clinically significant species within this genus is Blastomyces dermatitidis. These […]
[…] Testing: Enzyme immunoassays (EIAs) are commonly used to detect C. difficile toxins in stool samples. These toxins, especially […]
[…] Beyond anemia, MCH levels can provide insights into various medical conditions, ranging from nutritional deficiencies to chronic illnesses. […]
[…] When there is inadequate oxygen supply to tissues or cells, such as in cases of respiratory distress or poor circulation, lactate production can […]