HCV genotyping refers to determining the specific genotype or strain of the hepatitis C virus (HCV) infecting an individual. HCV is a highly variable virus with multiple genotypes and subtypes.
Genotyping is important for several reasons:
-
Treatment Selection:
Different HCV genotypes may respond differently to antiviral treatments. Knowing the genotype can help healthcare providers choose the most appropriate therapy for an infected individual. -
Disease Progression:
Some genotypes of HCV are associated with a higher risk of liver disease progression, such as cirrhosis and hepatocellular carcinoma. Genotyping can provide information about the potential severity of the infection. -
Epidemiological Studies:
HCV genotyping is also important for tracking the prevalence of different genotypes in various populations, which can aid in understanding the spread of the virus.
HCV genotyping is typically performed through molecular techniques that analyze the virus’s genetic material. The two main methods for HCV genotyping are:
-
Polymerase Chain Reaction (PCR):
PCR amplifies and analyzes specific regions of the HCV genome, typically the 5′ untranslated region (UTR) or the NS5B gene. The resulting genetic sequences are then compared to a reference database to determine the genotype and sometimes the subtype of the virus. -
Line Probe Assays:
Commercially available line probe assays, such as the INNO-LiPA HCV assay, can be used for genotyping. These assays use probes that bind to specific HCV genotypes, and the binding pattern indicates the genotype of the virus.
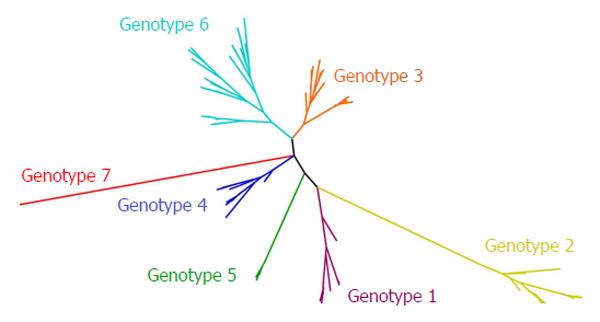
HCV is classified into several major genotypes (1-6) and numerous subtypes (e.g., 1a, 1b, 2a, 2b, etc.). Genotyping can identify which major genotype is present and, in some cases, the specific subtype. Different genotypes may require different treatment regimens, and knowing the subtype can provide further information about the virus’s characteristics.
Why do genotypes matter for treatment?
Here are several reasons why genotypes matter for treatment:
-
Drug Response:
Genotypes can influence how a person responds to medications. Some individuals may have genetic variations that make them more or less sensitive to certain drugs. For example, certain genetic variants can affect how quickly a drug is metabolized in the body, potentially leading to underdosing or overdosing if not considered in treatment planning. -
Drug Efficacy:
The effectiveness of a drug can vary based on an individual’s genotype. For some conditions, specific drug treatments may be more effective in individuals with particular genotypes. Tailoring treatment based on genotype can optimize therapeutic outcomes. -
Risk Assessment:
Genotypes can be used to assess an individual’s risk of developing certain diseases or conditions. For example, certain genetic markers are associated with an increased risk of developing cancer, heart disease, or other health issues. Knowing this information can help with early intervention and preventive measures. -
Personalized Medicine:
The concept of personalized medicine aims to customize medical treatments to an individual’s unique genetic profile. By understanding a patient’s genotype, healthcare providers can select the most appropriate treatments, dosages, and interventions, which can enhance treatment effectiveness and reduce the risk of adverse effects. -
Avoiding Adverse Reactions:
Some individuals may carry genetic variations that make them more prone to experiencing adverse reactions to specific drugs. Identifying these genetic factors in advance can help healthcare providers choose alternative treatments or adjust dosages to minimize the risk of adverse events. -
Precision Medicine:
Precision medicine is an approach that takes into account individual genetic variability to tailor medical interventions. Genotype information is crucial for the success of precision medicine, allowing for the development of targeted therapies that are more likely to work for a specific individual. -
Inherited Diseases:
Genotypes are particularly important when dealing with inherited or genetic disorders. Understanding the specific genetic mutations or variations responsible for a condition can guide treatment decisions and genetic counseling for affected individuals and their families. -
Clinical Trials:
Genotype information is often used in clinical trials to stratify participants and assess treatment responses in subpopulations. This can help identify which treatments are most effective for specific genotypes and contribute to the development of more targeted therapies.
Why do people have different genotypes?
People have different genotypes because of the way genetic inheritance works. Genotypes refer to the specific genetic makeup of an individual, which is determined by the combination of genes they inherit from their parents.
-
Genetic Variation:
Within a population, there is a natural variation in genes. This genetic diversity arises due to mutations, which are random changes in the DNA sequence. Mutations can occur spontaneously or be induced by environmental factors like radiation or chemicals. Over time, these mutations can accumulate and lead to different genetic variations in a population. -
Sexual Reproduction:
In sexually reproducing species, individuals inherit genetic material from both their mother and father. This process introduces additional variability because each parent contributes a unique set of genes to their offspring. As a result, siblings can have different genotypes, even though they share the same parents. -
Genetic Recombination
: During the formation of reproductive cells (sperm and eggs), a process called genetic recombination occurs. This involves the shuffling and exchange of genetic material between homologous chromosomes. Genetic recombination increases genetic diversity by creating novel combinations of alleles (different versions of a gene) in the offspring. -
Independent Assortment
: Humans have thousands of genes located on different chromosomes. When chromosomes segregate during meiosis (the process that forms sperm and eggs), they do so independently. This means that the assortment of genes onto each chromosome is random, leading to a wide range of possible genetic combinations in offspring. -
Random Chance
: At a fundamental level, the combination of genes from each parent is a matter of chance. For each gene, an individual has a 50% chance of inheriting the version (allele) from their mother and a 50% chance of inheriting the performance from their father. The combination of these probabilities results in a unique genotype for each individual. -
Genetic Drift:
In small populations, genetic drift can play a significant role in shaping genotypes. Genetic drift refers to the random fluctuations in allele frequencies due to chance events, which can lead to the loss or fixation of certain alleles in a population over generations. -
Natural Selection:
The environment also plays a role in shaping genotypes. Certain genetic variations may provide advantages or disadvantages in specific environments. Natural selection favors individuals with advantageous genotypes, leading to the propagation of those genotypes in a population.
Do genotypes change over time?
Genotypes themselves do not change over time within an individual organism’s lifetime. Genotypes are the genetic information or genetic code that an organism inherits from its parents, and they remain relatively stable throughout an individual’s life.
HARDER TO TREAT GENOTYPE 3:
Genotype 3 of the hepatitis C virus (HCV) has historically been considered more challenging to treat compared to some other genotypes, primarily due to its characteristics and response to standard antiviral therapies. However, it’s important to note that advancements in the field of hepatitis C treatment have led to improved outcomes for individuals with genotype 3 infections as well. Here are some key points to consider:
-
Genotype 3 Characteristics:
Genotype 3 is one of several genetic variations of the hepatitis C virus. It is associated with certain characteristics that have made it somewhat more challenging to treat, such as a higher rate of liver fibrosis progression, a higher likelihood of developing steatosis (fatty liver), and a lower response rate to traditional interferon-based therapies. -
Response to Treatment:
In the past, genotype 3 infections were often less responsive to the standard interferon-based treatments, resulting in lower sustained virologic response (SVR) rates. SVR means that the virus is undetectable in the blood and indicates a successful treatment outcome. -
Advancements in Treatment:
The landscape of hepatitis C treatment has evolved significantly with the development of direct-acting antiviral (DAA) drugs. DAAs have revolutionized the treatment of all genotypes of HCV, including genotype 3. These drugs are highly effective, have fewer side effects, and generally lead to high SVR rates, even for genotype 3 infections. -
Specific Regimens:
Specific DAA regimens are particularly effective for treating genotype 3. These regimens often include a combination of DAAs tailored to target the genotype 3 virus. Examples of DAAs used for genotype 3 treatment include sofosbuvir, daclatasvir, velpatasvir, and others. -
Duration of Treatment:
The duration of treatment for genotype 3 infections can vary depending on the specific DAA regimen and the individual patient’s characteristics. Some regimens may require 8 to 12 weeks of treatment, while others may extend to 16 weeks in certain cases. -
Monitoring and Follow-Up:
Regular monitoring during treatment and follow-up after treatment is important to assess treatment response and ensure that the virus is cleared from the body. This typically involves blood tests to check for the presence of HCV RNA and liver function. -
Consideration of Liver Disease:
The extent of liver damage or fibrosis may influence the choice of treatment regimen and the duration of treatment. Individuals with advanced liver disease may require more aggressive treatment approaches.
What tests are needed to know my genotype?
Determining your genotype involves identifying specific genetic variations or alleles you carry for particular genes or regions of your DNA. The tests required to determine your genotype can vary depending on the specific genes or genetic traits you want to examine. Here are some common methods and tests used to determine genotype:
-
Genetic Sequencing:
-
Whole Genome Sequencing (WGS):
This involves sequencing your entire genome to identify all the genetic variations and mutations you carry. It provides comprehensive information about your genotype but is also the most expensive option. -
Whole Exome Sequencing (WES):
WES focuses on sequencing the exons, which are the protein-coding regions of your genes. It is less expensive than WGS but still provides a significant amount of genetic information.
-
-
Genetic Panels:
-
Targeted Genetic Testing:
These panels focus on specific genes or genetic variations associated with particular conditions or traits. For example, you might opt for a panel that looks at genes related to breast cancer risk (BRCA1 and BRCA2) or pharmacogenomics (how your genes affect your response to medications).
-
-
Single Nucleotide Polymorphism (SNP) Testing:
-
SNP Genotyping:
This type of testing looks at specific SNPs, which are single-letter DNA variations that are known to be associated with certain traits or conditions. Companies like 23andMe use this approach for providing ancestry and health reports.
-
-
Sanger Sequencing:
This is a traditional DNA sequencing method used to determine the nucleotide sequence of a specific DNA fragment or gene. It’s less commonly used for personal genotyping but is still utilized in research and clinical settings. -
Polymerase Chain Reaction (PCR):
PCR is a technique used to amplify specific DNA regions, making it easier to analyze genetic variations in those regions. -
Fluorescent In Situ Hybridization (FISH):
FISH is used to detect and locate the presence or absence of specific DNA sequences or genes within a person’s chromosomes. -
Microarray Analysis:
This method involves using microarrays (small chips containing DNA probes) to analyze a person’s genetic material for specific variations or mutations. -
Molecular Genetic Testing:
This includes a range of techniques used to analyze specific genes, such as DNA sequencing, Southern blotting, and quantitative PCR. -
Genome-wide Association Studies (GWAS):
These large-scale studies examine the genomes of thousands of individuals to identify genetic variations associated with specific traits, diseases, or conditions. -
Parentage Testing:
These tests, such as paternity or maternity testing, determine genetic relationships between individuals by analyzing specific genetic markers.
To determine your genotype for a specific gene or condition, it’s important to consult with a healthcare professional or a genetic counselor who can recommend the most appropriate test based on your specific needs and medical history. Additionally, be aware that the availability and accuracy of genetic testing may vary depending on your location and the state of genetic testing technology at the time of testing.




[…] interpretation of blood chromosome test results depends on the specific findings observed during the chromosome analysis […]
[…] (AFP): AFP is a marker for liver cancer (hepatocellular carcinoma) and certain types of germ cell tumors. It can also be elevated in pregnancy and some […]
[…] the cervix. These changes may not produce noticeable symptoms but can be detected through cervical cancer screening tests, such as Pap smears or HPV tests. If left untreated, these changes can progress to […]