Cord blood Stem Cells
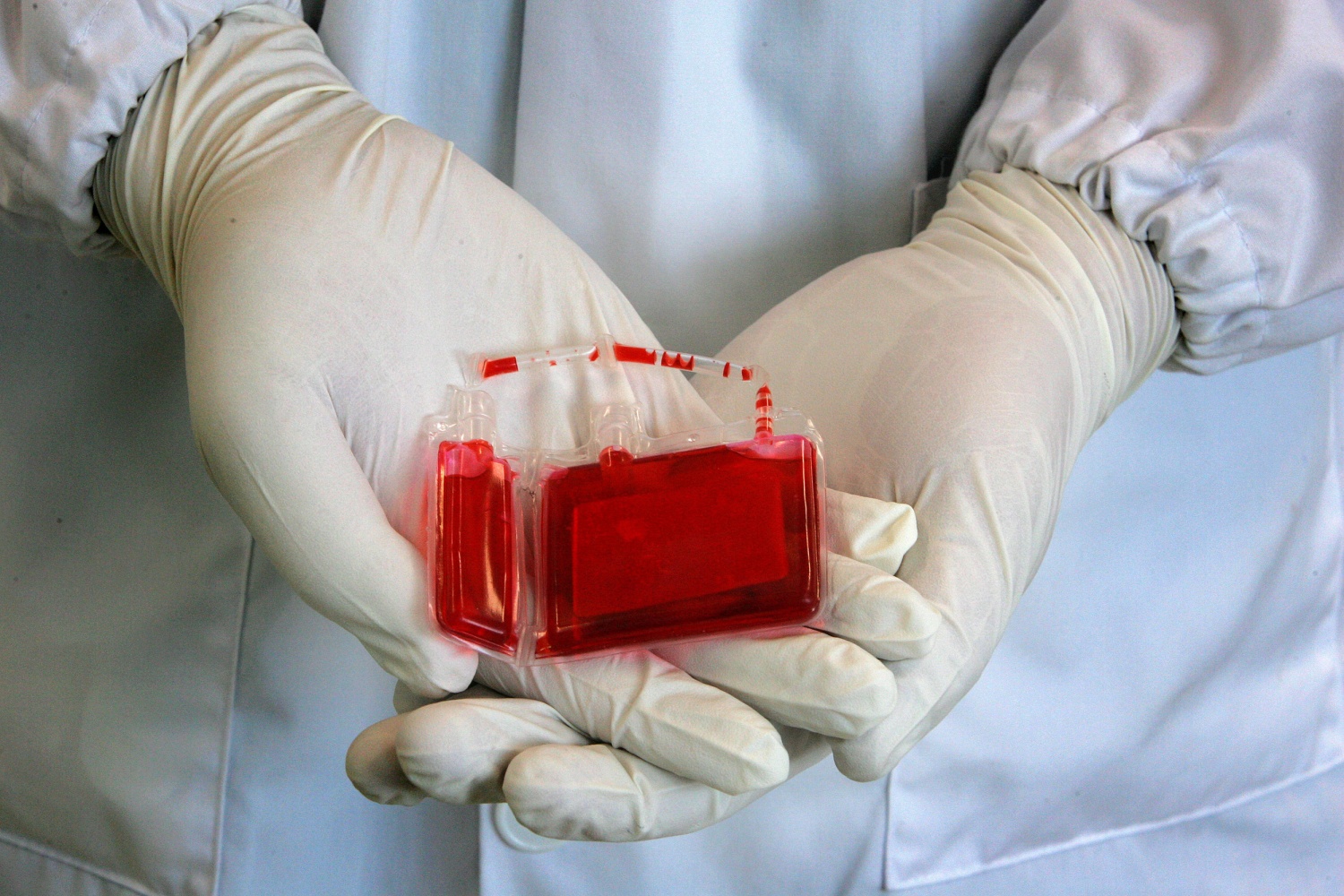
Cord blood is the blood that remains in the umbilical cord and placenta after a baby is born. It is collected shortly after birth and is rich in stem cells, specifically hematopoietic stem cells, which can develop into various types of blood cells, including red blood cells, white blood cells, and platelets.
Cord blood is valuable because it contains these stem cells, which can be used in medical treatments for a variety of conditions, including certain blood disorders, immune system disorders, and some genetic diseases. Stem cell transplantation from cord blood can be used as a treatment option for patients who require the replacement of damaged or diseased blood cells.
Cord blood banking is a process where parents can choose to have their baby’s cord blood collected, processed, and stored in a cord blood bank for potential future use. This is often done as an investment in case the child or a family member requires stem cell therapy later in life. Public cord blood banks also exist, where donated cord blood is made available for unrelated patients in need of stem cell transplantation.
Cord blood stem cells are particularly useful because they are less likely to cause graft-versus-host disease (GVHD) compared to other sources of stem cells, such as bone marrow. Additionally, they can often be used with less stringent tissue-matching requirements, making them a valuable resource in the field of regenerative medicine and transplantation.
What is cord blood banking used for?
Cord blood is rich in stem cells, specifically hematopoietic stem cells, which have the potential to develop into various types of blood cells, such as red blood cells, white blood cells, and platelets. These stem cells have several important medical applications:
- Treatment of Blood Disorders: Cord blood stem cells can be used to treat a wide range of blood disorders and diseases, including leukemia, lymphoma, and anemia. Stem cell transplants from cord blood can help replenish a patient’s damaged or diseased blood cells.
- Immune System Disorders: Stem cells from cord blood can be used in the treatment of immune system disorders like severe combined immunodeficiency (SCID) and other immune deficiencies. These stem cells can help rebuild a patient’s immune system.
- Metabolic Disorders: Some genetic metabolic disorders, such as Hurler syndrome and Krabbe disease, can be treated with cord blood stem cells. These stem cells can produce enzymes that are missing or defective in these disorders.
- Bone Marrow Failure Syndromes: Cord blood stem cell transplants can be a valuable treatment option for conditions where the bone marrow fails to produce enough blood cells, such as aplastic anemia.
- Regenerative Medicine: Research is ongoing into the use of cord blood stem cells for regenerative medicine purposes. They have the potential to repair damaged tissues and organs, making them a promising avenue for treating conditions like heart disease, stroke, and neurological disorders.
- Clinical Trials: Cord blood stem cells are also used in clinical trials to explore their potential for treating various diseases and conditions. Researchers are continually investigating new applications for these cells.
Cord blood banking can be done privately (for personal use by the baby or their family) or publicly (donated for use by anyone in need). Private cord blood banking allows families to preserve the cord blood for their potential future use, while public cord blood banking makes it available for anyone in need of a compatible match.
How do they find a match for stem cells from cord blood?
Finding a match for stem cells from cord blood, which is typically used for hematopoietic stem cell transplantation (HSCT) to treat various medical conditions like leukemia, lymphoma, and certain genetic disorders, involves a complex process that centers around human leukocyte antigen (HLA) typing. Here are the key steps involved in finding a suitable match:
- Cord Blood Collection: Cord blood is collected from the umbilical cord and placenta of a newborn immediately after birth. This blood is rich in hematopoietic (blood-forming) stem cells.
- Cord Blood Banking: The cord blood is sent to a cord blood bank for processing, testing, and long-term storage. The bank ensures that the cord blood is preserved in a manner that maintains the viability of the stem cells.
- HLA Typing: The next step is to determine the human leukocyte antigen (HLA) type of both the cord blood and the potential recipients. HLA is a set of genes that are involved in the immune system and plays a crucial role in compatibility. There are specific HLA markers that need to match between the donor (cord blood) and the recipient.
- HLA Matching: The goal is to find a cord blood unit that matches the recipient’s HLA type as closely as possible. A perfect match (10/10 match) is ideal, but a close match with fewer HLA disparities (9/10, 8/10 match) can also be considered depending on the specific medical condition and transplant protocol.
- Search Process: Cord blood banks maintain a database of HLA-typed cord blood units along with relevant information about the donors. When a transplant is needed, the medical team searches this database for suitable cord blood units. They look for a unit that matches the recipient’s HLA type to the greatest extent possible.
- Selection: Once a potential match is identified, the medical team assesses other factors such as the number of stem cells in the unit, the age of the unit, and any other relevant information to determine if it’s a suitable choice for transplantation.
- Confirmation: Before transplantation, the selected cord blood unit undergoes further testing and confirmation to ensure its quality and compatibility.
- Transplantation: If a suitable match is found, the cord blood unit is prepared and transplanted into the recipient, similar to a bone marrow transplant. The infused stem cells then have the potential to regenerate the recipient’s blood and immune system.
Public cord blood banking:
Public cord blood banking involves the collection, storage, and maintenance of umbilical cord blood units from newborns for use in medical treatments and research. Here’s an overview of public cord blood banking:
-
Collection Process
Cord blood is collected from the umbilical cord and placenta immediately after childbirth. The process is safe and painless for both the mother and the baby. The blood is drawn into a collection bag or vial. -
Processing and Storage
After collection, the cord blood is processed in a lab to remove red blood cells and other contaminants. The remaining stem cells are then frozen and stored in a cord blood bank. -
Public vs. Private Cord Blood Banking:
- Public Cord Blood Banking: In the public system, donated cord blood is made available to anyone in need of a stem cell transplant. It is usually donated voluntarily by parents who do not have a specific need for their baby’s cord blood. The donated cord blood is listed on a registry and can be accessed by patients worldwide.
- Private Cord Blood Banking: In the private system, parents pay to have their baby’s cord blood stored exclusively for their family’s use. This is done in case a family member needs a stem cell transplant in the future. Private banks charge an initial fee for collection and storage and often an annual storage fee.
- Uses:
- Public Cord Blood Banking: Cord blood collected in public banks is primarily used for treating patients with various diseases, such as leukemia, lymphoma, and certain genetic disorders, who require stem cell transplants. It is a valuable resource for individuals who do not have a compatible donor in their family.
- Private Cord Blood Banking: The cord blood stored in private banks is reserved for the donor child or their family. It can potentially be used in the treatment of certain diseases or conditions, but this is less common than using it for public donations.
- Ethical Considerations: Public cord blood banking is often encouraged because it promotes equity and availability of stem cell treatments to a wider population. Private cord blood banking is a personal choice but comes with costs and the possibility that the stored cord blood may never be needed.
- Regulation: Public cord blood banks are typically regulated by government health agencies to ensure safety and quality standards are met. Private cord blood banks are also subject to regulations but may have varying levels of oversight depending on the jurisdiction.
- Donation Process: If parents choose to donate their baby’s cord blood to a public bank, they typically need to pre-register and inform their healthcare provider about their intent. The collection process is then coordinated by the bank.
- Availability: Access to cord blood from public banks is typically available to anyone in need who is a suitable match, whereas access to privately stored cord blood is limited to the family that stored it.
Public cord blood banking has proven to be a valuable resource for treating various medical conditions, and it plays a crucial role in providing potentially life-saving stem cell transplants to patients around the world.
Private cord blood banking:
Private cord blood banking is a process where parents or guardians choose to store their baby’s umbilical cord blood and tissue for potential future medical use, typically for the child or family members. This is done through a private cord blood bank, also known as a family cord blood bank. Here’s how it works:
- Collection: During childbirth, medical professionals collect the baby’s umbilical cord blood and tissue after the baby is born and the umbilical cord is clamped and cut. This process is painless and poses no risk to the baby or the mother.
- Processing and Storage: The collected cord blood and tissue are processed to isolate and preserve the stem cells present within them. These stem cells are then cryogenically frozen and stored in specialized storage facilities.
- Ownership: The stored cord blood and tissue are owned by the baby or, in some cases, the parents or guardians. It is important to clarify the ownership and legal aspects of the chosen private cord blood bank.
- Potential Uses:
- Autologous Use: The stored cord blood and tissue can be used by the child from whom it was collected, should they require stem cell treatments for certain medical conditions in the future.
- Family Use: Cord blood and tissue can also be used by compatible family members, such as siblings, parents, or grandparents, if they have a matching tissue type and require stem cell therapy.
- Costs: Private cord blood banking typically involves an initial collection and processing fee, followed by annual storage fees. These costs can vary significantly between different cord blood banks.
- Medical Advances: The decision to bank cord blood privately is often driven by the hope of potential medical advances that may harness stem cells for treating various diseases and conditions, including certain cancers, genetic disorders, and blood disorders. However, it’s important to note that the use of stored cord blood is not a guaranteed cure for any specific ailment.
- Public Cord Blood Banking: An alternative to private cord blood banking is public cord blood donation. In this case, parents can choose to donate their baby’s cord blood to a public cord blood bank, where it becomes available for anyone in need of a stem cell transplant. This is done free of charge and can potentially help save lives.
Before deciding on private cord blood banking, parents need to weigh the costs, benefits, and potential risks associated with this decision. They should also consult with healthcare professionals to make an informed choice that aligns with their family’s medical history and needs.
When do I need to decide about cord blood banking?
The decision about cord blood banking should ideally be made well before your baby’s due date, as it involves some planning and paperwork. Here are some key considerations and a general timeline to help you make this decision:
- Early Pregnancy (First Trimester):
- Start researching cord blood banking options and gather information about different cord blood banks in your region.
- Consult with your healthcare provider about cord blood banking to get their input and recommendations.
- Consider your family’s medical history and whether any hereditary diseases might make cord blood banking a more valuable option for your family.
- Mid-Pregnancy (Second Trimester):
- Narrow down your choices of cord blood banks based on your research and consultations with healthcare professionals.
- Contact the selected cord blood bank(s) to get detailed information about their services, costs, and the logistics involved.
- Third Trimester (Late Pregnancy):
- Make a final decision about cord blood banking and complete the necessary paperwork.
- Notify your healthcare provider and the birthing facility about your decision, as they will need to be prepared for the collection process.
- Birth Day:
- Ensure that your cord blood collection kit is ready and available to take to the hospital or birthing center.
- Inform the medical staff of your decision to bank cord blood so they can facilitate the collection process.
- After Birth:
- Cord blood collection typically occurs immediately after the baby is born and the umbilical cord is cut. The process is performed by trained healthcare professionals or cord blood bank representatives.
- The collected cord blood is then transported to the chosen cord blood bank for processing and storage.

How is cord blood collected?
Cord blood is a rich source of hematopoietic stem cells, which can be used in the treatment of various diseases, including certain types of cancer, blood disorders, and immune system disorders. Here’s how cord blood collection typically takes place:
- Preparation: The collection process begins with the healthcare provider informing the expectant parents about cord blood banking options and obtaining their consent if they choose to proceed with the collection.
- Timing: Cord blood is collected shortly after the baby is born, usually within 5 to 10 minutes after delivery. It’s important to collect the cord blood quickly to ensure the highest quality and quantity of stem cells.
- Sterilization: The healthcare provider ensures that all equipment and materials used for cord blood collection are sterile to minimize the risk of contamination.
- Identification: The umbilical cord is clamped and cut as it normally would be during a standard childbirth procedure. One end of the cord is attached to the baby, and the other end is attached to the placenta. The healthcare provider identifies the portion of the cord attached to the placenta for collection.
- Cord Blood Collection: There are two main methods for collecting cord blood:
- In-utero collection: This method involves collecting the cord blood while the baby is still attached to the placenta inside the mother’s womb. A needle is inserted into the umbilical vein, and the blood is drawn into a collection bag via gravity.
- Ex-utero collection: In this method, the healthcare provider clamps the cord close to the baby and then cuts it. The cord blood is collected from the exposed end of the cord after it has been clamped. This is the more common method.
- Blood Transfer: The collected cord blood is transferred into a sterile collection bag or container specifically designed for cord blood banking. The bag is usually equipped with an anticoagulant to prevent the blood from clotting.
- Labeling and Documentation: The bag containing the cord blood is carefully labeled with the mother’s and baby’s identification information. All relevant documentation, including consent forms and medical records, is completed.
- Transport and Storage: The cord blood is then transported to a cord blood bank, where it undergoes processing, testing, and long-term cryopreservation in liquid nitrogen storage tanks.
How is cord blood stored?
Here is an overview of the steps involved in collecting and storing cord blood:
- Collection: Cord blood is collected immediately after the baby is born, and the umbilical cord is clamped and cut. There are two main methods for collecting cord blood:
- In utero collection: In this method, a needle is inserted into the umbilical vein before the placenta is delivered. The blood is then drawn into a collection bag.
- Ex utero collection: This method involves collecting the cord blood after the placenta has been delivered. A needle is inserted into the umbilical vein, and the blood is collected in a bag.
- Processing: After collection, the cord blood is processed in a lab to separate the stem cells from the rest of the blood components. This typically involves centrifugation to concentrate the stem cells.
- Testing: The cord blood is tested for various infectious diseases, including HIV and hepatitis, to ensure that it is safe for transplantation.
- Cryopreservation: Once the cord blood has been processed and tested, it is frozen and stored at extremely low temperatures, typically in liquid nitrogen. This cryopreservation process helps to preserve the viability of the stem cells for many years.
- Storage: Cord blood can be stored in private or public cord blood banks. Private cord blood banks store cord blood for the family’s personal use, while public cord blood banks store it for use by anyone in need of a stem cell transplant who matches the donor’s cord blood.
Is cord blood banking free?
Cord blood banking is not typically free. It involves the collection, processing, and storage of a newborn’s umbilical cord blood, which contains valuable stem cells that can be used in medical treatments. Cord blood banking services are usually offered by private companies, and they charge fees for the collection and storage of cord blood.
The cost of cord blood banking can vary significantly depending on the company and the specific services offered. It’s essential to research different cord blood banking providers, compare their pricing, and understand the terms and conditions of their services before making a decision.
Some factors that can affect the cost of cord blood banking include whether you choose public or private banking, the length of storage, and any additional services or insurance options you may select. Public cord blood banks may offer free or low-cost banking for donation purposes, but these cord blood units are typically made available to the public for transplant and research purposes rather than being reserved for private use.
If you are interested in cord blood banking, it’s advisable to contact cord blood banking companies directly to get the most up-to-date pricing information and to discuss your specific needs and options. Keep in mind that the cost of cord blood banking is an investment in potential future medical treatments or therapies for your child or family members, should the need arise.


Search for Quality Bali Real Estate
Gain Your Freedom with Bali Villas for Sale
The Perfect Place to Live
Make your investments in Bali
[…] base of the brain. It plays a crucial role in the growth, development, and maintenance of various tissues and organs in the human body. Here are some key functions and aspects of growth […]
[…] Evaluates the breakdown of red blood cells and liver […]
[…] Screening: In many countries, newborns are routinely screened for sickle cell disease shortly after birth. This involves collecting a […]
[…] which is a mechanism to repair the defects in DNA which leads to chromosomal breaks this leads to stem cell depletion one of those famous stem cells are the […]