Antibiotic Resistance Gene, Antibiotic Resistance means when an antibiotic drug on medicines does not work against infection in the body and worsens over time. or the types of bacteria that come from the environment, and are already exposed to a particular antibiotic in the human body.
Sometimes this antibiotic resistance is against a Particular antibiotic, sometimes it is against Some antibiotics and sometimes it can be against
all antibiotics.
Causes of Antibiotic Resistance:
- Use of Antibiotics in incomplete doses.
- Using antibiotics without a doctor’s advice.
- Excessive use of antibiotics even when they are not needed.
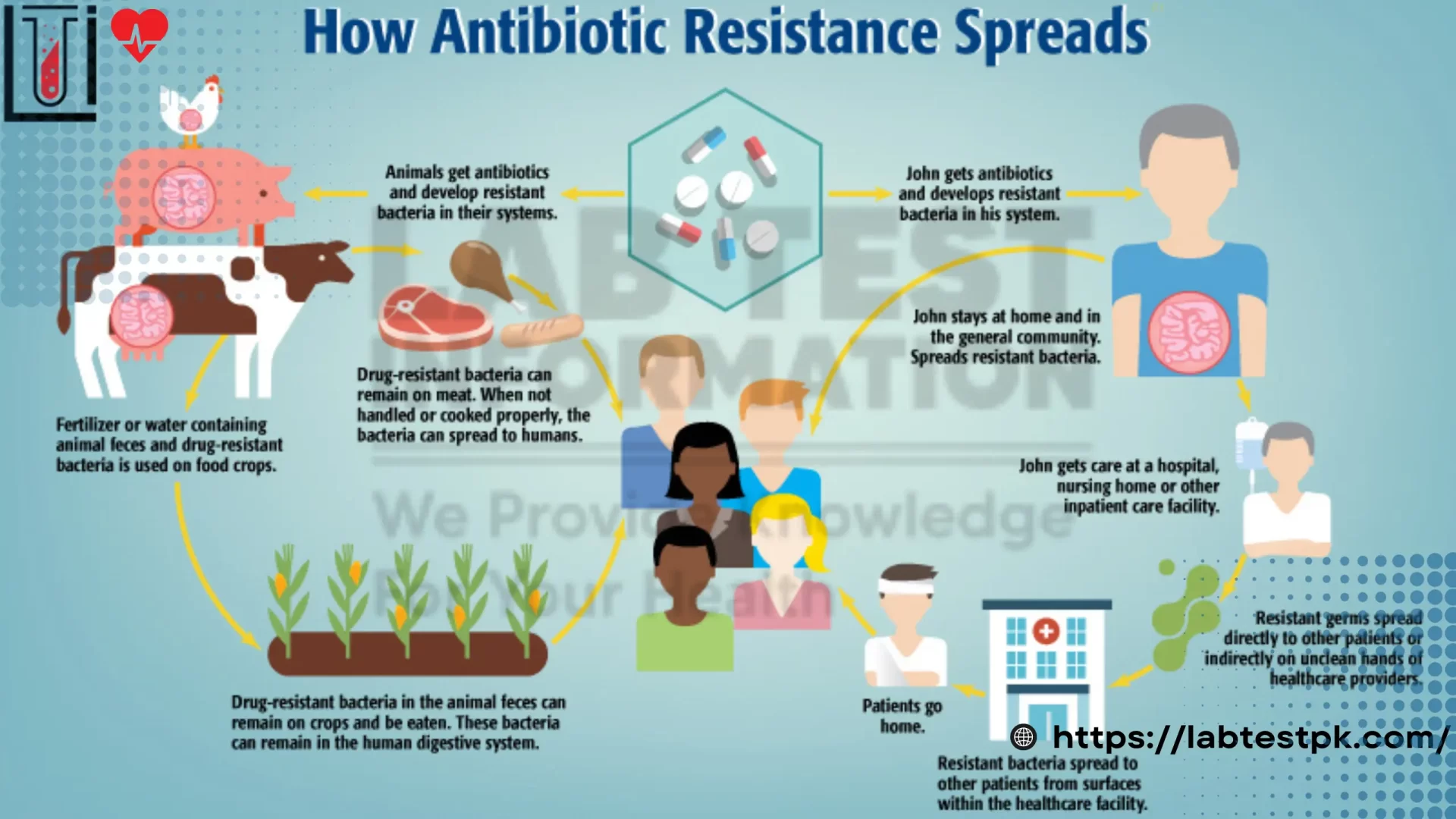
- Use of antibiotics in animals whose Products are consumed by humans.
- Changing the DNA of bacteria in its structure against antibiotics.
- A bacterial infection is transmitted from Person who is already infected with antibiotic resistance.
Diagnosis:
- Culture and Sensitivity Test.
- Rapid Tests for Specific Infections that Recurrent.
Types of Antibiotic Resistance (Antibiotic Resistance Gene)
They have 4 Categories of antibiotic Resistance:
- Inactivating drug
- Limiting uptake of drug
- Modifying drug target
- Active ding efflux
-
Intrinsic Resistance:
- This is a natural resistance that all bacteria of a particular species possess. It is due to the inherent structural or functional characteristics of the bacteria. For example, Gram-negative bacteria have an outer membrane that acts as a barrier to many antibiotics.
-
Acquired Resistance:
- This occurs when bacteria acquire resistance through mutations in their genetic material or by obtaining resistance genes from other bacteria. Acquired resistance can be further divided into:
- Mutational Resistance: Spontaneous mutations in the bacterial genome can lead to changes that reduce the effectiveness of antibiotics.
- Horizontal Gene Transfer: Bacteria can acquire resistance genes from other bacteria through mechanisms such as transformation (uptake of naked DNA), transduction (bacteriophage-mediated transfer), and conjugation (direct transfer of DNA through cell-to-cell contact).
- This occurs when bacteria acquire resistance through mutations in their genetic material or by obtaining resistance genes from other bacteria. Acquired resistance can be further divided into:
-
Mechanism-Based Resistance:
- Bacteria can resist antibiotics through several specific mechanisms:
- Enzymatic Degradation: Bacteria produce enzymes that chemically modify and inactivate the antibiotic. For example, beta-lactamases break down beta-lactam antibiotics.
- Efflux Pumps: Bacteria have proteins that actively pump antibiotics out of the cell, reducing the intracellular concentration of the drug to sub-lethal levels.
- Target Modification: Bacteria alter the antibiotic’s target site, so the drug can no longer bind effectively. For example, mutations in ribosomal proteins can confer resistance to macrolides.
- Reduced Permeability: Bacteria alter their cell membrane to prevent the antibiotic from entering the cell. This is common in Gram-negative bacteria due to changes in porin proteins.
- Bacteria can resist antibiotics through several specific mechanisms:
-
Cross-Resistance:
- This occurs when resistance to one antibiotic confers resistance to other antibiotics, typically those within the same class or with similar mechanisms of action. For example, resistance to one aminoglycoside may confer resistance to other aminoglycosides.
-
Multiple Drug Resistance (MDR):
- Bacteria that are resistant to multiple antibiotics are referred to as MDR. These bacteria can resist treatment with several different types of antibiotics, making infections difficult to treat.
-
Extensively Drug-Resistant (XDR):
- Bacteria that are resistant to nearly all antibiotics may still be susceptible to one or two classes of antibiotics.
-
Pandrug-Resistant (PDR):
- Bacteria that are resistant to all available antibiotics, leaving no options for effective antimicrobial therapy.
Understanding these types of antibiotic resistance is crucial for developing new strategies to combat bacterial infections and mitigate the spread of resistant strains.

[…] Bone marrow trephine biopsy(b) Liver biopsy(d) Serum ferritin ✓(d) Serum LDH levels(e) Total iron binding […]
I cling on to listening to the newscast lecture about getting free online grant applications so I have been looking around for the most excellent site to get one. Could you advise me please, where could i acquire some?
[…] Ristocetin is an antibiotic that induces platelet aggregation by causing it to bind to von Willebrand factor, a protein […]
[…] Tests: These are the most common and can detect recent drug use within a few days to a few weeks, depending on the […]