Adrenocorticotrophic Hormone (ACTH), also known as corticotropin, is a hormone produced and secreted by the anterior pituitary gland in the brain. It plays a crucial role in regulating the body’s stress response and the function of the adrenal glands.
Here are some key functions and aspects of Adrenocorticotrophic Hormone (ACTH):
- Stimulation of Adrenal Glands: ACTH’s primary role is to stimulate the adrenal cortex, which is the outer portion of the adrenal glands. This stimulation results in the release of various hormones, particularly glucocorticoids, including cortisol. Cortisol is essential for various physiological processes, such as metabolism, immune response, and the body’s response to stress.
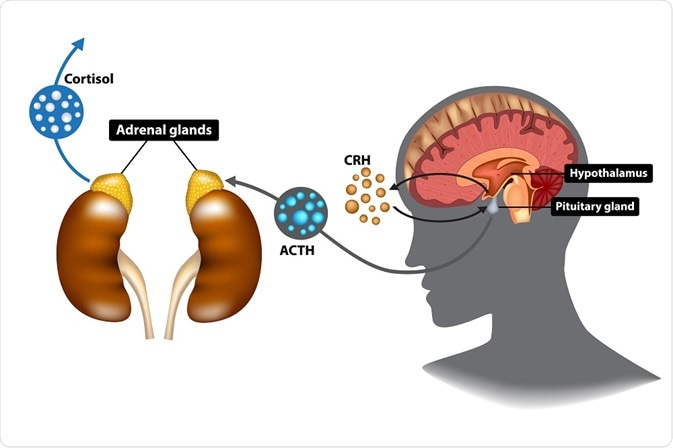
- Stress Response: When the body encounters stress, whether physical or emotional, the hypothalamus-pituitary-adrenal (HPA) axis is activated. The hypothalamus releases corticotropin-releasing hormone (CRH), which, in turn, stimulates the pituitary gland to release ACTH. ACTH then prompts the adrenal glands to produce cortisol. Cortisol helps the body cope with stress by increasing energy production and reducing inflammation.
- Circadian Rhythm: ACTH secretion follows a diurnal (daily) pattern, with higher levels in the morning and lower levels in the evening. This rhythmic release of ACTH contributes to the body’s natural wake-sleep cycle.
- Feedback Control: The release of ACTH is regulated by a negative feedback loop. Elevated cortisol levels in the blood signal the hypothalamus and pituitary gland to reduce the production of CRH and ACTH, preventing excessive cortisol secretion.
- Medical Uses: Synthetic forms of ACTH can be used for diagnostic purposes and in the treatment of certain medical conditions, such as Addison’s disease (adrenal insufficiency), or testing the responsiveness of the adrenal glands.
- Testing: ACTH stimulation tests are often conducted to assess the function of the adrenal glands. In this test, a synthetic form of ACTH is administered, and cortisol levels in the blood are measured to determine the adrenal gland’s response.
Excessive or insufficient levels of ACTH can lead to various health problems. High levels of ACTH can be associated with conditions like Cushing’s disease, which leads to excessive cortisol production. In contrast, low levels of ACTH can be linked to Addison’s disease, characterized by adrenal insufficiency.
Overall, ACTH is a critical hormone that helps the body respond to stress and maintain various physiological processes. Its regulation is essential for overall health and well-being.
What is the function of adrenocorticotropic hormone (ACTH)?
Here’s how ACTH functions in the body:
- Regulation of Cortisol Production: ACTH primarily regulates the production of cortisol in the adrenal cortex. Cortisol is a steroid hormone that plays a crucial role in various physiological processes, including regulating metabolism, immune response, blood pressure, and the body’s response to stress.
- Stress Response: In times of physical or psychological stress, the hypothalamus in the brain releases corticotropin-releasing hormone (CRH), which, in turn, stimulates the release of ACTH from the anterior pituitary. Elevated ACTH levels result in increased cortisol production, which helps the body respond to stress by mobilizing energy resources and suppressing the immune system temporarily.
- Circadian Rhythm: ACTH and cortisol secretion follow a diurnal (daily) rhythm, with the highest levels typically occurring in the morning and the lowest levels at night. This circadian pattern helps regulate various physiological processes, including sleep-wake cycles and energy metabolism.
- Immune Function: ACTH and cortisol have immunosuppressive effects, which can be beneficial during times of stress to prevent the immune system from overreacting. However, chronic or excessive production of cortisol due to dysregulation of the H
- PA (hypothalamic-pituitary-adrenal) axis can lead to immune system dysfunction.
How are ACTH levels controlled?
Here’s how ACTH levels are controlled:
- Hypothalamus: The process begins in the hypothalamus, which is a region in the brain. The hypothalamus senses changes in the body’s internal environment, including stress, low blood sugar, and other factors that may require an increase in cortisol production. In response to these stimuli, the hypothalamus releases corticotropin-releasing hormone (CRH) into the bloodstream.
- Pituitary Gland: CRH travels through the bloodstream to the anterior pituitary gland, another structure in the brain. Upon detecting the presence of CRH, the pituitary gland secretes ACTH.
- Adrenal Glands: ACTH then travels through the bloodstream to the adrenal glands, which are small glands located on top of each kidney. In response to ACTH, the adrenal glands release cortisol into the bloodstream. Cortisol is a stress hormone that has a wide range of effects on the body, including increasing blood sugar levels and suppressing the immune system.
- Negative Feedback: As cortisol levels in the bloodstream rise, they send signals back to the hypothalamus and the pituitary gland, indicating that the body has sufficient cortisol. This results in a reduction in the release of CRH and ACTH. This negative feedback loop helps to maintain stable cortisol levels in the body.
- Stress Response: In times of stress, the HPA axis is activated to increase cortisol production. This is part of the body’s “fight or flight” response, which prepares the body to respond to stressors. Once the stressor is resolved, the HPA axis returns to its baseline state.
What test checks ACTH levels?
The test that checks adrenocorticotropic hormone (ACTH) levels in the body is called the ACTH blood test. This test measures the amount of ACTH in your blood and is typically used to diagnose or monitor conditions related to the adrenal glands, such as Cushing’s syndrome and Addison’s disease. ACTH is a hormone produced by the brain’s pituitary gland It stimulates the adrenal glands to produce cortisol, a hormone that plays a key role in various bodily functions. Abnormal levels of ACTH can be indicative of various medical conditions, and the test helps healthcare providers make accurate diagnoses and treatment decisions.
What are normal ACTH levels?
ACTH (Adrenocorticotropic Hormone) levels in the blood can vary depending on the time of day and various factors. Normal reference ranges for ACTH levels can also differ slightly between different laboratories and assays, so it’s important to interpret the results in the context of the specific reference range used by the testing facility.
However, in a typical reference range, normal fasting ACTH levels are often in the range of 10 to 60 picograms per milliliter (pg/mL). These levels can vary, and they tend to be highest in the morning and lower in the evening.
What happens when ACTH levels are high?
Here are some common conditions and situations that can lead to elevated ACTH levels and their associated effects:
- Cushing’s Syndrome: One of the most common causes of high ACTH levels is Cushing’s syndrome. This condition is characterized by excessive cortisol production, which can result in various symptoms, including weight gain, high blood pressure, muscle weakness, mood swings, and a characteristic “moon face.”
- Pituitary Adenoma: A tumor in the pituitary gland can lead to overproduction of ACTH, causing increased cortisol levels. This can result in Cushing’s syndrome, as mentioned above.
- Ectopic ACTH Production: Sometimes, tumors outside of the pituitary gland, such as in the lungs or other organs, can produce ACTH. This can lead to elevated cortisol levels and Cushing’s syndrome.
- Stress: High stress levels can temporarily increase ACTH secretion and, consequently, cortisol levels. While this is a normal stress response, chronic stress can have adverse effects on health over time.
- Certain Medications: Some medications, such as corticosteroids, can lead to increased ACTH levels due to feedback mechanisms in the body. Prolonged use of these medications can cause Cushing’s syndrome-like symptoms.
The symptoms and consequences of high ACTH levels are primarily related to excess cortisol production. Long-term, elevated cortisol levels can lead to a range of health issues, including:
- Weight gain, especially around the abdomen.
- High blood pressure.
- Muscle and bone weakness.
- Mood changes, such as anxiety and depression.
- Skin problems, like thinning and easy bruising.
- Impaired immune function.
- Increased risk of infections.
- Osteoporosis (bone thinning).
The underlying cause of high ACTH levels will determine the appropriate treatment. It may involve surgery to remove tumors, discontinuing medication, or other interventions to regulate cortisol production. It’s essential to consult with a healthcare professional for a proper diagnosis and treatment plan if you suspect you have high ACTH levels or related symptoms.
What happens when ACTH levels are low?
Here are some of the key consequences of low ACTH levels:
- Decreased cortisol production: ACTH stimulates the adrenal glands to produce cortisol, a hormone that is essential for various bodily functions, including regulating metabolism, immune response, and the body’s response to stress. When ACTH levels are low, cortisol production is reduced.
- Fatigue and weakness: Cortisol helps maintain blood sugar levels, and low cortisol levels can lead to low blood sugar, which can result in symptoms like fatigue, weakness, and dizziness.
- Low blood pressure: Cortisol also plays a role in regulating blood pressure. Low cortisol levels can lead to decreased blood pressure, potentially causing symptoms like dizziness and even fainting.
- Weight loss and appetite changes: Cortisol affects the metabolism of carbohydrates, proteins, and fats. Low cortisol levels can lead to weight loss and changes in appetite.
- Gastrointestinal symptoms: Low cortisol levels can lead to nausea, vomiting, and abdominal pain.
- Reduced immune function: Cortisol is an important regulator of the immune system. Low cortisol levels can result in a weakened immune response, making the individual more susceptible to infections and illnesses.
- Skin changes: Cortisol affects the skin, and low cortisol levels can lead to changes such as darkening of the skin (hyperpigmentation), particularly in skin creases and scars.
Low ACTH levels can result from various conditions, including:
- Pituitary gland dysfunction: A tumor, injury, or other issues affecting the pituitary gland can result in reduced ACTH production.
- Adrenal insufficiency: Conditions such as Addison’s disease, which primarily affects the adrenal glands, can lead to low ACTH levels.
- Medications: Some medications, like corticosteroids, can suppress the production of ACTH and cortisol.
Treatment for low ACTH levels typically involves addressing the underlying cause. For example, in cases of adrenal insufficiency, hormone replacement therapy with synthetic cortisol (glucocorticoids) may be necessary to replace the missing cortisol.




[…] a class of central nervous system (CNS) stimulant drugs that affect the brain and body. They are synthetic compounds chemically similar to the naturally occurring substances found in the human body, such as […]
[…] Anti-Adrenal Antibody, Anti-adrenal antibodies are autoantibodies that target components of the adrenal glands, which are part of the endocrine system and are responsible for producing hormones like cortisol and adrenaline. These antibodies can be associated with autoimmune disorders that affect the adrenal glands, such as autoimmune Addison’s disease. […]
[…] Test is a form of prolactin, a hormone produced by the pituitary gland in the brain. Prolactin plays a crucial role in the regulation of […]
[…] Problem with Pituitary Gland […]
[…] Adrenal Insufficiency: This condition is brought on by insufficient pituitary production of adrenocorticotropic hormone (ACTH), which lowers adrenal gland stimulation and, as a result, lowers levels of adrenal […]
[…] diet high in sugar, refined carbohydrates, and processed foods can promote candida […]
[…] of food poisoning are self-limiting and mild, causing, symptoms like abdominal pain, diarrhea, vomiting, and […]
[…] are disrupted, leading to a range of symptoms and complications, including neurological issues, skin problems, and hair loss. A biotinidase test can help diagnose this condition in infants and […]